| Original Article | ||
Open Vet J. 2023; 13(3): 262-269 Open Veterinary Journal, (2023), Vol. 13(3): 262–269 Short Communication Comparison of patellar position and moment arm between tibial plateau leveling osteotomy and cranial closing wedge ostectomy: An ex vivo studyMasakazu Shimada*, Sawako Murakami, Takahisa Tanigawa, Nobuo Kanno, Yasuji Harada and Yasushi HaraDivision of Veterinary Surgery, Department of Veterinary Science, Faculty of Veterinary Medicine, Nippon Veterinary and Life Science University, Tokyo, Japan *Corresponding Author: Masakazu Shimada. Division of Veterinary Surgery, Department of Veterinary Science, Faculty of Veterinary Medicine, Nippon Veterinary and Life Science University, Tokyo, Japan. Email: masakazu42710 [at] gmail.com. Submitted: 13/10/2022 Accepted: 05/02/2023 Published: 03/03/2023 © 2023 Open Veterinary Journal
AbstractBackground: Tibial plateau leveling osteotomy (TPLO) and cranial closing wedge ostectomy (CCWO) are common treatments for cranial cruciate ligament disease. These two techniques mainly differ in whether the proximal tibial fragment contains the attachment site of the patellar ligament. Currently, no reports compare how these techniques affect the patellofemoral joint. Aim: This ex vivo study aimed to compare the effects of TPLO and CCWO on the patellar position and moment arm in healthy Beagles. Methods: TPLO and CCWO were performed on each stifle in six cadavers of Beagles. Pre- and postoperative mediolateral radiographs with the stifle angle at approximately 90° were obtained. The modified Blumensaat index (MBI), patellar ligament length to patella length ratio (PLL:PL), and patellar moment arm (PMA) were measured in each radiograph. Mixed-model multiple regression analyses for the MBI, PLL:PL, and PMA, with the surgical procedure as the independent variable, were then performed. The joint angle was included as an independent variable for MBI and PMA. Results: The PLL:PL was decreased after TPLO. Additionally, the PLL:PL after TPLO was significantly lower than that after CCWO. The MBI decreased with flexion. Postoperative MBI values were reduced for both procedures, with lower values after CCWO than after TPLO. The PMA values decreased with flexion. Postoperative values for both methods were reduced in the PMA, with the values being lower after CCWO than after TPLO. Conclusion: Both TPLO and CCWO affect the patellofemoral joint. Compared with TPLO, CCWO produced more excellent downward traction on the patella. Therefore, CCWO may be used to correct the patellar alta and treat cranial cruciate ligament disease. Keywords: Cranial cruciate ligament disease, Tibial plateau leveling osteotomy, Cranial closing wedge ostectomy, Patellofemoral joint. IntroductionMost canine cranial cruciate ligament (CrCL) ruptures are associated with ligamentous degeneration characterized by chondrometaplasia, which is also known as “cranial cruciate ligament disease (CCLD)” (Hayashi et al., 2004). Although the exact pathophysiology remains unclear, it is thought to involve cranial tibial thrust (CrTT) during weight-bearing (Slocum and Devine, 1983; Cook, 2010; Comerford et al., 2011). CrCL inhibits cranial tibial displacement and prevents excessive internal rotation and extension (Arnoczky and Marshall, 1977; Shimada et al., 2020). Consequently, complete CrCL ruptures result in tibial subluxation cranially with weight-bearing. There has been increasing use of functional stabilization, which prevents tibial subluxation by neutralizing the CrTT, to allow rapid recovery of postoperative gait (Oxley et al., 2013; Bergh et al., 2014; Campbell et al., 2016; Krotscheck et al., 2016). Procedures for functional stabilization include cranial closing wedge ostectomy (CCWO) and tibial plateau leveling osteotomy (TPLO) (Slocum and Devine, 1984; Slocum and Slocum, 1993; Kim et al., 2008; Christ et al., 2018). Both techniques neutralize CrTT by reducing the tibial plateau angle (TPA); however, there are differences in the postoperative tibial morphology between these two procedures (Kim et al., 2008; Guénégo et al., 2021). In particular, significant differences result from whether or not the proximal tibial fragment contains the attachment site of the patellar ligament. Therefore, the surgical effect on the patella and patellar ligament varies across different techniques. The patella acts as an extension of the moment arm of the stifle extensor mechanism unit and as a lever that converts the contractile force of the quadriceps muscles into a force during extension (Dan et al., 2018). It is thus important to evaluate the patellofemoral joint when considering stifle flexion and extension motion. Patellar alta and baja are abnormalities of the patella position related to the femoral trochlea and associated with patellar luxation (Mostafa et al., 2008; Biedert and Tscholl, 2017). In addition, the position of the patella significantly affects the stifle joint flexion (Johnson et al., 2002). In human medicine, the Insall-Salvati index, which is minimally affected by flexion and extension, is among the most common measurement used in diagnosing patellar alta (Biedert and Tscholl, 2017). Veterinary medicine has applied a similar measurement to the Insall-Salvati index known as the patellar ligament length to patella length ratio (PLL:PL) (Johnson et al., 2002, 2006; Mostafa et al., 2008; Murakami et al., 2021). Unfortunately, the PLL:PL cannot directly assess the patellar position relative to the femoral trochlea. Moreover, given the biomechanical properties of the patellar ligament, which can be considered rigid (Bennett et al., 2022), osteotomy-related length changes are expected to be small. Therefore, the PLL:PL may be an inappropriate measure for the morphological comparison of the pre-and postoperative patellofemoral joint. In the veterinary field, the proximal and distal patellar positions (PPP and DPP, respectively) are used to evaluate the patellar position relative to the femoral trochlea (Murakami et al., 2021; Johnson et al., 2002). However, PPP and DPP are not direct measures of the patellar height as they can be affected by changes in other degrees of freedom of the patella, such as patellar tilt and rotation. In human medicine, the modified Blumensaat index (MBI) is used to evaluate patellar height using the ratio of the distance from the Blumensaat line to the midpoint at the patellofemoral joint of the patella against the length of the Blumensaat line exists (Hanada et al., 2014). Therefore, we incorporated the MBI as measurements for objectively assessing the patellar height based on the surgical technique.
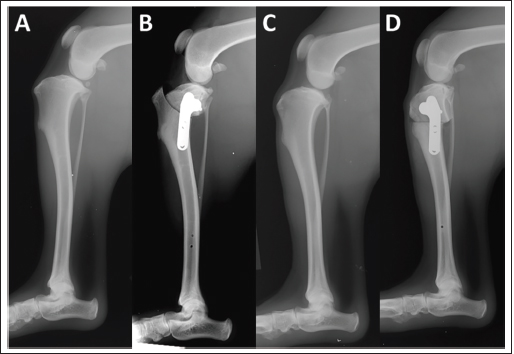
Fig. 1. Mediolateral stifle radiography. Preoperative (A) and postoperative (B) radiographs of TPLO in the same stifle joint and preoperative (C) and postoperative (D) radiographs of CCWO in the same stifle joint.
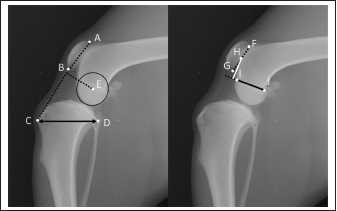
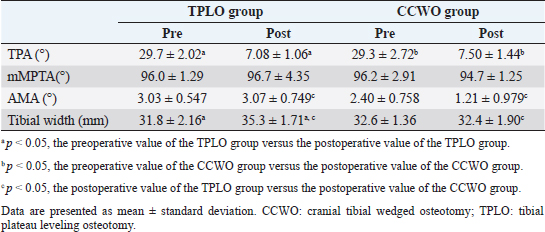
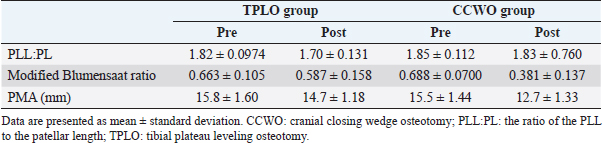
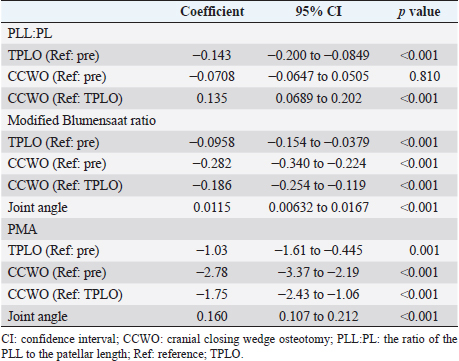
Fig. 2. Measurement method. The patellar length was calculated by dividing the patellar ligament length (distance from point B to C) by the patellar length (distance from point A to B). Tibial width was defined as the distance from point C to D. The PMA was defined as the distance between point E and the intersection point of a perpendicular line from point E to line BC. The distance from the Blumensaat line (line IJ) to the midpoint at the patellofemoral joint of the patella (distance from point F to G) was defined as α (white line). The length of the Blumensaat line (distance from the point I to J) was defined as β (black line). α/β were defined as MBI. A: patella base, B: patella apex, C: tibial tuberosity, D: caudal end of the tibial plateau, E: femoral condyle center, F: the proximal point of the patellofemoral joint of the patella, G: the distal point of the patellofemoral joint of the patella, H: the midpoint at the patellofemoral joint of the patella, I: cranial point of the Blumensaat line, J: caudal point of the Blumensaat line. The patellar moment arm (PMA) is defined as the perpendicular distance between the patellar ligament force vector and the center of the tibiofemoral joint and is involved in the biomechanics of the stifle joint. Changes in quadriceps force associated with changes in PMA may be engaged in patellar ligament thickening, and biomechanical investigations of the moment arm changes with TPLO or tibial tuberosity advancement and quadriceps force have been conducted in the past (Guerrero et al., 2011; Dan et al., 2019; Kanno et al., 2019). Previous studies have demonstrated that TPLO and CCWO both lower the patellar position; however, there have been no comparisons of the effect on the patellofemoral joint between these two procedures (Guénégo et al., 2021). Additionally, no studies have directly evaluated the patellofemoral joint as described above. Therefore, we hypothesized that compared with TPLO, CCWO produces greater downward traction on the patella. To investigate this hypothesis, this study aimed to compare the surgical outcomes of CCWO and TPLO procedures on each limb in the same dog. Materials and MethodsAnimalsSix cadavers from healthy uncastrated male Beagle dogs that had been euthanized and used for soft-tissue surgery training for veterinary students were used in this study. The cadaver specimens had undergone abdominal and thoracic incisions and sutures during student practice; however, the hind limbs, including soft tissues, had not been manipulated. In addition, the included subjects lacked orthopedic abnormalities on palpation before euthanasia. Specimen preparationPreoperative mediolateral radiographs with the tibiofemoral and tarsal joints at approximately 90° and craniocaudal radiographs were obtained. The TPA was measured on the mediolateral image. The reported optimal TPAs for TPLO and CCWO are 6.5° ± 0.9° and 3.8° ± 2.0° to 5.9° ± 3.0°, respectively (Warzee et al., 2001; Apelt et al., 2010), with no significant difference between the two techniques. Therefore, we standardized the preoperative planning with a target postoperative TPA of 6.5° for techniques as in a previous report (Warzee et al., 2001). In each dog, CCWO was performed on one side, as described by a previous report by Christ et al. (2018), while TPLO was performed on the opposite side, as described by Slocum and Slocum (1993). A medial approach was applied. After the arthrotomy, intra-articular structures, including the cruciate ligament and meniscus, were confirmed grossly to be expected, and the joint capsule was sutured. After jig placement, osteotomy was performed based on the preoperative plan. Subsequently, fixation was done using a 2.4-mm diameter TPLO plate (Johnson & Johnson, NJ, USA) in each procedure (Fig. 1). Finally, postoperative radiographs in the mediolateral and the craniocaudal view were obtained as previously described. Radiographic evaluationThe joint angle, TPA, anatomical-mechanical angle (AMA), PLL:PL, MBI, and PMA were measured from the mediolateral radiographs of the stifle joint (Fig. 2). The joint angle was defined as the angle formed by the anatomical axes of the femur and distal tibia. The AMA was defined as the angle formed by the distal tibial anatomy and the tibial mechanical axis, as Guénégo et al. (2017) reported. Tibial width was defined as the distance from the patellar ligament insertion of the tibia to the caudal end of the tibial plateau. The PLL:PL was calculated by dividing the PLL, which is the length from the most distal point on the patella to the patellar ligament insertion on the tibial tuberosity, by the PL, which is the length from the patella base to the patella apex, as described by Mostafa et al. (2008). The MBI was measured as described by Hanada et al. (2014). The distance from the Blumensaat line to the midpoint at the patellofemoral joint of the patella was defined as α. The length of the Blumensaat line was determined as β. MBI was defined as α/β. PMA was defined as the distance from the center of the femoral condyle to an intersection point of the perpendicular line and from the femoral condyle center to the patellar ligament, as described by Pozzi et al. (2013). We also measured the mechanical medial proximal tibial angle (mMPTA) from the craniocaudal image described by Dismukes et al. (2007). All radiographic images were randomized and measured by one person (MS). All measurements were performed using computer-aided design software (AR_CAD v1.6.0; SHF Co., Kyoto, Japan). Statistical analysisStatistical analyses were performed using Stata (version 14, StataCorp). Shapiro-Wilk test confirmed normal data distribution. Therefore, we used parametric tests. Between-group differences in postoperative changes in the TPA, mMPTA, AMA, and TW were evaluated using repeated-measures analysis of variance. Additionally, Scheffe’s method was used as a post hoc analysis. Mixed-model multiple regression analyses of PLL:PL, MBI, and PMA, with the surgical procedure as the independent variable, were performed. Previous studies have demonstrated that MBI and PMA, but not PLL:PL, are affected by the stifle joint angle (Hanada et al., 2015; Johnson et al., 2002; Pozzi et al., 2013). Therefore, the joint angle was included as an independent variable for MBI and PMA. A unique number for each dog was included as a random repeated effect. Statistical significance was set at p < 0.05. Ethical approvalThe study protocol was approved by our university’s Animal Experiment Committee and Bioethics Committee (approval number: 2019S-59). ResultsThe mean weight and age of the included dogs were 12.4 ± 1.0 kg and 16.3 ± 2.4 months, respectively. There were no significant between-group differences in the pre-and postoperative TPA and mMPTA (Preoperative: TPA, p=0.782; mMPTA, p=0.909; Postoperative: TPA, p=0.470; mMPTA, p=0.346). There was a postoperative decrease in the AMA after CCWO (p=0.057) but not after TPLO (p=0.922). The postoperative AMA values were significantly lower after CCWO than after TPLO (p=0.007). In addition, there was a postoperative increase in the tibial width after TPLO (p=0.018) (Table 1). There was a postoperative decrease in the PLL:PL after TPLO (p < 0.001) but not after CCWO, with the PLL:PL values being significantly lower after TPLO than after CCWO (p < 0.001) (Tables 2 and 3). The MBI values significantly decreased with flexion (p < 0.001). In addition, there was a postoperative decrease in the MBI after both procedures (CCWO; p < 0.001, TPLO; p < 0.001). Furthermore, the MBI values were significantly lower after CCWO than after TPLO (p < 0.001) (Tables 2 and 3). The PMA values decreased with flexion (p < 0.001). There was also a postoperative decrease in the PMA after both procedures (CCWO; p < 0.001, TPLO; p=0.001), with the PMA values being lower after CCWO than after TPLO (p < 0.001) (Tables 2 and 3). DiscussionOur findings showed that compared with TPLO, CCWO produced greater downward traction on the patella, thus confirming our hypothesis. Although TPLO also had a downward traction effect on the patella, its impact was significantly smaller than that of CCWO. Guenego et al. (2021) reported that TPLO and CCWO had a downward traction effect on the patella. However, they did not use the same measurement method for TPLO and CCWO. Moreover, they did not perform between-technique comparisons. In contrast, our findings suggest that based on the MBI, CCWO exerted greater downward traction on the patella than TPLO. The between-technique differences could be attributed to these two factors. As shown in Figure 3, TPLO does not move the origin of the patellar tendon; however, CCWO displaces it downward, which could have significantly affected the patellar position. Moreover, the intercondylar ridge position cranially shifts in CCWO, which results in decreased AMA values. These changes in the proximal tibial morphology could have also affected the PMA. In a review of tibial tuberosity advancement and TPLO conducted by Dan et al. (2019), tibial tuberosity advancement was found to have significantly less patellar ligament thickening than TPLO, which was attributed to the increase in quadriceps muscle force related to the decrease in PMA. In our study, CCWO led to smaller PMA values than TPLO, which, as Dan et al. (2019) suggested, increased the risk of subsequent thickening of the patellar ligament after CCWO. Guenego et al. (2021) reported that, unlike TPLO, CCWO rarely showed postoperative thickening of the patellar ligament. In addition to biomechanical changes in the patellofemoral joint, various factors could be involved in patellar ligament thickening, including impaired blood flow to the patellar ligament ligaments such as that caused by arthroscopy/arthrotomy and osteotomy, irritation of the patellar ligament during osteotomy, and postoperative activity of the dog (Pacchiana et al., 2003; Carey et al., 2005; Johnson et al., 2016). Therefore, factors other than PMA may be involved in patellar tendon thickening. Table 1. Values of parameters in each group.
Table 2. Values of stifle parameters in each group.
Table 3. Multiple regression analysis for each stifle joint parameter.
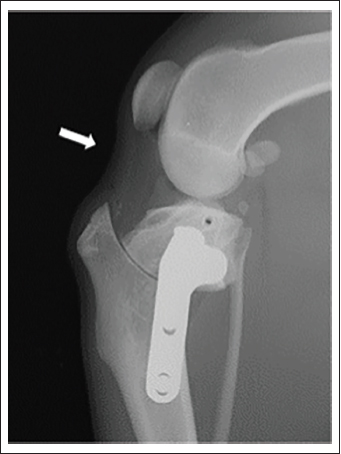
In our study, TPLO demonstrated downward traction of the patella but to a lesser extent than CCWO. Previous studies have reported decreasing PLL:PL value after TPLO (Guénégo et al., 2021). In an ex vivo study, Pozzi et al. (2013) reported the effects of TPLO on the patellofemoral joint, including the distal and caudal displacement of the patella relative to the femur as well as a decreased patellar tilt angle. Additionally, Jay et al. (2019) reported a postoperative decrease in the PLL. Specifically, the change in the PLL could have led to the downward traction of the patella, which could be attributed to the shortening of the distance between radiological landmarks rather than the actual shortening of the PLL. In our study, there was a postoperative caudal deflection of the patellar ligament (Fig. 4). As shown in Figure 3, the tibia widens as the bone rotates, and the cranial side of the proximal fragment sinks downward in TPLO. Consequently, the patellar ligament and surrounding soft tissues may have been pulled and deflected. In addition, a change in the patellar axis may have occurred with patellar ligament deflection, as Pozzi et al. (2013) reported, which may have affected the PLL. Consequently, the patella was considered to have moved mildly downward.
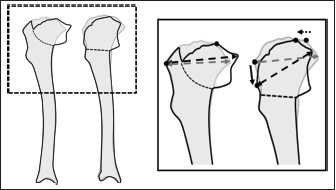
Fig. 3. Changes in proximal morphology associated with osteotomy. The radiographs were traced and compared preoperatively (grey line) and postoperatively (black line). The tibial tuberosity position changes in CCWO but not in TPLO; moreover, the tibial tuberosity is displaced downward (black, solid arrow). The position of the intercondylar eminence changes cranially in CCWO (black and dotted arrows). The tibial width changes after TPLO (both arrows). CCWO: TPLO. Patellar alta may be among the pathologies of medial patellar luxation (Mostafa et al., 2008). In addition, medial patellar luxation could be a factor in CCLD, especially in small dogs (Campbell et al., 2010; Spinella et al., 2021). Accordingly, there are scattered cases of concomitant CCLD and medial patellar luxation, and patellar alta may occur among these cases. Among the techniques for medial patellar luxation with patellar alta is the transition of the tibial tuberosity to the external-distal aspect (Segal et al., 2012). Downward traction of the patella with tibial tuberosity displacement is considered among the most effective methods for patellar alta. Talaat et al. (2006) reported that CCWO could be expected to cause downward traction on patellar elevation, which is consistent with our findings. However, compared with TPLO, CCWO has been less explored.
Fig. 4. Deflection of the patellar ligament. Mediolateral radiograph of the stifle joint after TPLO. The patellar ligament is caudally deflected (white arrow). TPLO. Favorable results have been reported for both CCWO and TPLO based on the incidence of postoperative complications in clinical cases and postoperative evaluation. However, these were done by administering questionnaires to owners and thus were subjective evaluations (Corr and Brown, 2007; Oxley et al., 2013). One study reported that CCWO increased the angular velocity of the stifle joint in extension and may cause hyperextension of the stifle joint during the swing phase (Lee et al., 2007). Positional changes in the patella and alterations in the PMA may influence gait. On radiographs, the distal tibial axis is used to measure joint angles. The proximal joint angles are variable and could affect the gait. Therefore, our findings do not provide sufficient insight into the effects of downward displacement by CCWO, even in clinical settings. Future studies are warranted to clarify the effects of each surgical technique on the patellofemoral joint, including gait analysis. These findings could inform the future case-based selection of surgical techniques for CCLD. This study has several limitations. First, this was a cadaver study. In clinical cases, the patellar position may change with muscle tension. Thus, the results of this study could differ in actual clinical settings. Second, we only used one Beagle breed, which may have anatomical differences from other breeds. Third, this was an exploratory study with a limited number of available specimens, which limits the statistical significance of our specimens. In summary, our study found that compared with TPLO, CCWO has a more significant downward traction effect on the patella. Our findings may inform treatment choices in cases involving patellar alta. Nonetheless, future clinical studies are necessary to elucidate the impact of each osteotomy. AcknowledgmentsWe gratefully acknowledge the work of past and present members of the Division of Veterinary Surgery of Nippon Veterinary and Life Science University. We also thank Editage (www.editage.com) for English language editing. Conflict of interestNo third-party funding or support was received in connection with this study or the writing or publication of the manuscript. The authors declare that there is no conflict of interest. FundingThe authors declare that Masakazu Shimada received funding from an AO VET Seed Grant (No. 115492) outside the submitted work in the past. None of the authors of this manuscript has a financial or personal relationship with people or organizations that could inappropriately influence or bias its contents. ReferencesApelt, D., Pozzi, A., Marcellin-Little, D.J. and Kowaleski, M.P. 2010. Effect of cranial tibial closing wedge angle on tibial subluxation: an ex vivo study. Vet. Surg. 39, 454–459. Arnoczky, S.P. and Marshall, J.L. 1977. The cruciate ligaments of the canine stifle: an anatomical and functional analysis. Am. J. Vet. Res. 38, 1807–1814. Bennett, K., Vincent, T. and Sakthi-Velavan, S. 2022. The patellar ligament: A comprehensive review. Clin. Anat. 35, 52–64. Bergh, M.S., Sullivan, C., Ferrell, C.L., Troy, J. and Budsberg, S.C. 2014. Systematic review of surgical treatments for cranial cruciate ligament disease in dogs. J. Am. Anim. Hosp. Assoc. 50, 315–321. Biedert, R.M. and Tscholl, P.M. 2017. Patella alta: a comprehensive review of current knowledge. Am. J. Orthop. (Belle Mead NJ) 46, 290–300. Campbell, C.A., Horstman, C.L., Mason, D.R. and Evans, R.B. 2010. Severity of patellar luxation and frequency of concomitant cranial cruciate ligament rupture in dogs: 162 cases (2004-2007). J. Am. Vet. Med. Assoc. 236, 887–891. Campbell, K.A., Payne, J.T., Doornink, M.T. and Haggerty, J. 2016. Outcome of tibial closing wedge osteotomy in 55 cranial cruciate ligament-deficient stifles of small dogs (<15 kg). Vet. Surg. 45, 1056–1062. Carey, K., Aiken, S.W., DiResta, G.R., Herr, L.G. and Monette, S. 2005. Radiographic and clinical changes of the patellar tendon after tibial plateau leveling osteotomy 94 cases (2000-2003). Vet. Comp. Orthop. Traumatol. 18, 235–242. Christ, J.P., Anderson, J.R. and Youk, A.O. 2018. Modified cranial closing wedge ostectomy in 25 dogs. Vet. Surg. 47, 683–691. Comerford, E.J., Smith, K. and Hayashi, K. 2011. Update on the aetiopathogenesis of canine cranial cruciate ligament disease. Vet. Comp. Orthop. Traumatol. 24, 91–98. Cook, J.L. 2010. Cranial cruciate ligament disease in dogs: biology versus biomechanics. Vet. Surg. 39, 270–277. Corr, S.A. and Brown, C. 2007. A comparison of outcomes following tibial plateau levelling osteotomy and cranial tibial wedge osteotomy procedures. Vet. Comp. Orthop. Traumatol. 20, 312–319. Dan, M., Parr, W., Broe, D., Cross, M. and Walsh, W.R. 2018. Biomechanics of the knee extensor mechanism and its relationship to patella tendinopathy: a review. J. Orthop. Res. 36, 3105–3112. Dan, M.J., Crowley, J., Broe, D., Cross, M., Tan, C. and Walsh, W.R. 2019. Patella tendinopathy Zoobiquity - What can we learn from dogs? Knee. 26, 115–123. Dismukes, D.I., Tomlinson, J.L., Fox, D.B., Cook, J.L. and Song, K.J. 2007. Radiographic measurement of the proximal and distal mechanical joint angles in the canine tibia. Vet. Surg. 36, 699–704. Guénégo, L., Payot, M., Charru, P. and Verwaerde, P. 2017. Comparison of tibial anatomical-mechanical axis angle between predisposed dogs and dogs at low risk for cranial cruciate ligament rupture. Vet. J. 225, 35–41. Guénégo, L., Vezzoni, A. and Vezzoni, L. 2021. Comparison of tibial anatomical-mechanical axis angles and patellar positions between tibial plateau levelling osteotomy (TPLO) and modified cranial closing wedge osteotomy (AMA-based CCWO) for the treatment of cranial cruciate ligament disease in large dogs with tibial plateau slopes greater than 30 degrees and clinically normal Labradors retrievers. BMC Vet. Res. 17, 368. Guerrero, T.G., Pozzi, A., Dunbar, N., Kipfer, N., Haessig, M., Beth Horodyski, M., and Montavon, P.M. 2011. Effect of tibial tuberosity advancement on the contact mechanics and the alignment of the patellofemoral and femorotibial joints. Vet. Surg. 40, 839–848. Hanada, M., Takahashi, M., Koyama, H., and Matsuyama, Y. 2014. Comparison of the change in patellar height between opening and closed wedge high tibial osteotomy: measurement with a new method. Eur. J. Orthop. Surg. Traumatol. 24, 567–570. Hanada, M., Takahashi, M., Koyama, H., and Matsuyama, Y. 2015. Assessing the validity of the modified Blumensaat method for radiographic evaluation of patellar height. Eur. J. Orthop. Surg. Traumatol. 25, 757–762. Hayashi, K., Manley, P.A. and Muir, P. 2004. Cranial cruciate ligament pathophysiology in dogs with cruciate disease: a review. J. Am. Anim. Hosp. Assoc. 40, 385–390. Jay, M.R., Mattoon, J.S., Gilbert, P.J., Tanaka, T.T. and Beaty, B.L. 2019. Radiographic evaluation of patellar ligament length after tibial plateau leveling osteotomy in dogs. Am. J. Vet. Res. 80, 607-612. Johnson, A.L., Broaddus, K.D., Hauptman, J.G., Marsh, S., Monsere, J. and Sepulveda, G. 2006. Vertical patellar position in large-breed dogs with clinically normal stifles and large-breed dogs with medial patellar luxation. Vet. Surg. 35, 78–81. Johnson, A.L., Probst, C.W., DeCamp, C.E., Rosenstein, D.S., Hauptman, J.G. and Kern, T.L. 2002. Vertical position of the patella in the stifle joint of clinically normal large-breed dogs. Am. J. Vet. Res. 63, 42–46. Johnson, M.D., Shmon, C.L., Linn, K.A. and Singh, B. 2016. Ex vivo evaluation of the effect of various surgical procedures on blood delivery to the patellar tendon of dogs. Am. J. Vet. Res. 77, 548–555. Kanno, N., Ochi, Y., Ichinohe, T., Hakozaki, T., Suzuki, S., Harada, Y., Yogo, T., and Hara, Y. 2019. Effect of the centre of rotation in tibial plateau levelling osteotomy on quadriceps tensile force: an ex vivo study in canine cadavers. Vet. Comp. Orthop. Traumatol. 32, 117–125. Kim, S.E., Pozzi, A., Kowaleski, M.P. and Lewis, D.D. 2008. Tibial osteotomies for cranial cruciate ligament insufficiency in dogs. Vet. Surg. 37, 111–125. Krotscheck, U., Nelson, S.A., Todhunter, R.J., Stone, M. and Zhang, Z. 2016. Long term functional outcome of tibial tuberosity advancement vs. tibial plateau leveling osteotomy and extracapsular repair in a heterogeneous population of dogs. Vet. Surg. 45, 261–268. Lee, J.Y., Kim, G., Kim, J.H. and Choi, S.H. 2007. Kinematic gait analysis of the hind limb after tibial plateau levelling osteotomy and cranial tibial wedge osteotomy in ten dogs. J. Vet. Med. A Physiol. Pathol. Clin. Med. 54, 579–584. Mostafa, A.A., Griffon, D.J., Thomas, M.W. and Constable, P.D. 2008. Proximodistal alignment of the canine patella: radiographic evaluation and association with medial and lateral patellar luxation. Vet. Surg. 37, 201–211. Murakami, S., Shimada, M., Harada, Y. and Hara, Y. 2021. Examination of the proximodistal patellar position in small dogs in relation to anatomical features of the distal femur and medial patellar luxation. PLoS One. 16, e0252531. Oxley, B., Gemmill, T.J., Renwick, A.R., Clements, D.N. and McKee, W.M. 2013. Comparison of complication rates and clinical outcome between tibial plateau leveling osteotomy and a modified cranial closing wedge osteotomy for treatment of cranial cruciate ligament disease in dogs. Vet. Surg. 42, 739–750. Pacchiana, P.D., Morris, E., Gillings, S.L., Jessen, C.R. and Lipowitz, A.J. 2003. Surgical and postoperative complications associated with tibial plateau leveling osteotomy in dogs with cranial cruciate ligament rupture: 397 cases (1998-2001). J. Am. Vet. Med. Assoc. 222, 184–193. Pozzi, A., Dunbar, N.J. and Kim, S.E. 2013. Effect of tibial plateau leveling osteotomy on patellofemoral alignment: a study using canine cadavers. Vet. J. 198, 98–102. Segal, U., Or, M. and Shani, J. 2012. Latero-distal transposition of the tibial crest in cases of medial patellar luxation with Patella alta. Vet. Comp. Orthop. Traumatol. 25, 281–285. Shimada, M., Takagi, T., Kanno, N., Yamakawa, S., Fujie, H., Ichinohe, T., Suzuki, S., Harada, Y. and Hara, Y. 2020. Biomechanical effects of tibial plateau levelling osteotomy on joint instability in normal canine stifles: an in vitro study. Vet. Comp. Orthop. Traumatol. 33, 301–307. Slocum, B. and Devine, T. 1983. Cranial tibial thrust: a primary force in the canine stifle. J. Am. Vet. Med. Assoc. 183, 456–459. Slocum, B. and Devine, T. 1984. Cranial tibial wedge osteotomy: a technique for eliminating cranial tibial thrust in cranial cruciate ligament repair. J. Am. Vet. Med. Assoc. 184, 564–569. Slocum, B. and Slocum, T.D. 1993. Tibial plateau leveling osteotomy for repair of cranial cruciate ligament rupture in the canine. Vet. Clin. North Am. Small Anim. Pract. 23, 777–795. Spinella, G., Arcamone, G. and Valentini, S. 2021. Cranial cruciate ligament rupture in dogs: review on biomechanics, etiopathogenetic factors and rehabilitation. Vet. Sci. 8, 186. Talaat, M.B., Kowaleski, M.P. and Boudrieau, R.J. 2006. Combination tibial plateau leveling osteotomy and cranial closing wedge osteotomy of the tibia for the treatment of cranial cruciate ligament-deficient stifles with excessive tibial plateau angle. Vet. Surg. 35, 729–739. Warzee, C.C., Dejardin, L.M., Arnoczky, S.P. and Perry, R.L. 2001. Effect of tibial plateau leveling on cranial and caudal tibial thrusts in canine cranial cruciate-deficient stifles: an in vitro experimental study. Vet. Surg. 30, 278–286. | ||
| How to Cite this Article |
| Pubmed Style MS, Murakami S, Tanigawa T, Kanno N, Harada Y, Hara Y. Comparison of patellar position and moment arm between tibial plateau leveling osteotomy and cranial closing wedge ostectomy: An ex vivo study. Open Vet J. 2023; 13(3): 262-269. doi:10.5455/OVJ.2023.v13.i3.2 Web Style MS, Murakami S, Tanigawa T, Kanno N, Harada Y, Hara Y. Comparison of patellar position and moment arm between tibial plateau leveling osteotomy and cranial closing wedge ostectomy: An ex vivo study. https://www.openveterinaryjournal.com/?mno=113569 [Access: May 01, 2024]. doi:10.5455/OVJ.2023.v13.i3.2 AMA (American Medical Association) Style MS, Murakami S, Tanigawa T, Kanno N, Harada Y, Hara Y. Comparison of patellar position and moment arm between tibial plateau leveling osteotomy and cranial closing wedge ostectomy: An ex vivo study. Open Vet J. 2023; 13(3): 262-269. doi:10.5455/OVJ.2023.v13.i3.2 Vancouver/ICMJE Style MS, Murakami S, Tanigawa T, Kanno N, Harada Y, Hara Y. Comparison of patellar position and moment arm between tibial plateau leveling osteotomy and cranial closing wedge ostectomy: An ex vivo study. Open Vet J. (2023), [cited May 01, 2024]; 13(3): 262-269. doi:10.5455/OVJ.2023.v13.i3.2 Harvard Style , M. S., Murakami, . S., Tanigawa, . T., Kanno, . N., Harada, . Y. & Hara, . Y. (2023) Comparison of patellar position and moment arm between tibial plateau leveling osteotomy and cranial closing wedge ostectomy: An ex vivo study. Open Vet J, 13 (3), 262-269. doi:10.5455/OVJ.2023.v13.i3.2 Turabian Style , Masakazu Shimada, Sawako Murakami, Takahisa Tanigawa, Nobuo Kanno, Yasuji Harada, and Yasushi Hara. 2023. Comparison of patellar position and moment arm between tibial plateau leveling osteotomy and cranial closing wedge ostectomy: An ex vivo study. Open Veterinary Journal, 13 (3), 262-269. doi:10.5455/OVJ.2023.v13.i3.2 Chicago Style , Masakazu Shimada, Sawako Murakami, Takahisa Tanigawa, Nobuo Kanno, Yasuji Harada, and Yasushi Hara. "Comparison of patellar position and moment arm between tibial plateau leveling osteotomy and cranial closing wedge ostectomy: An ex vivo study." Open Veterinary Journal 13 (2023), 262-269. doi:10.5455/OVJ.2023.v13.i3.2 MLA (The Modern Language Association) Style , Masakazu Shimada, Sawako Murakami, Takahisa Tanigawa, Nobuo Kanno, Yasuji Harada, and Yasushi Hara. "Comparison of patellar position and moment arm between tibial plateau leveling osteotomy and cranial closing wedge ostectomy: An ex vivo study." Open Veterinary Journal 13.3 (2023), 262-269. Print. doi:10.5455/OVJ.2023.v13.i3.2 APA (American Psychological Association) Style , M. S., Murakami, . S., Tanigawa, . T., Kanno, . N., Harada, . Y. & Hara, . Y. (2023) Comparison of patellar position and moment arm between tibial plateau leveling osteotomy and cranial closing wedge ostectomy: An ex vivo study. Open Veterinary Journal, 13 (3), 262-269. doi:10.5455/OVJ.2023.v13.i3.2 |