| Research Article | ||
Open Vet. J.. 2025; 15(8): 3677-3683 Open Veterinary Journal, (2025), Vol. 15(8): 3677-3683 Research Article Sporotrichosis incidence and risk factors in cats in Thonburi District, Bangkok, Thailand: A retrospective studyNarong Kulnides1*, Athip Lorsirigool1,2, Natapol Pumipuntu3, Nontachai Santichat4, Kanokwan Tawinwang5, Arunroj Kullaya6, Wirongrong Thamyo7 and Rachada Fongtanakit81Department of Forensic Science, Graduate School, Suan Sunandha Rajabhat University, Bangkok, Thailand 2TerdThai Love Pet Clinic, Bangkok, Thailand 3One Health Research Unit, Faculty of Veterinary Science, Mahasarakham University, Maha Sarakham, Thailand 4Department of Livestock Development, Udon Thani Animal Quarantine Station, Udon, Thailand 5Tepin Pet Clinic, Nong Bua Lamphu, Thailand 6Faculty of Veterinary Science, Mahasarakham University, Maha Sarakham Thailand 7Faculty of Science and Technology, Suan Sunandha Rajabhat University, Bangkok, Thailand 8Doctor of Philosophy Program in Development Administration, Suan Sunandha Rajabhat University, Bangkok, Thailand *Corresponding Author: Narong Kulnides. Department of Forensic Science, Graduate School, Suan Sunandha Rajabhat University, Bangkok, Thailand. Email: narong.ku [at] ssru.ac.th Submitted: 09/06/2025 Revised: 19/07/2025 Accepted: 22/07/2025 Published: 31/08/2025 © 2025 Open Veterinary Journal
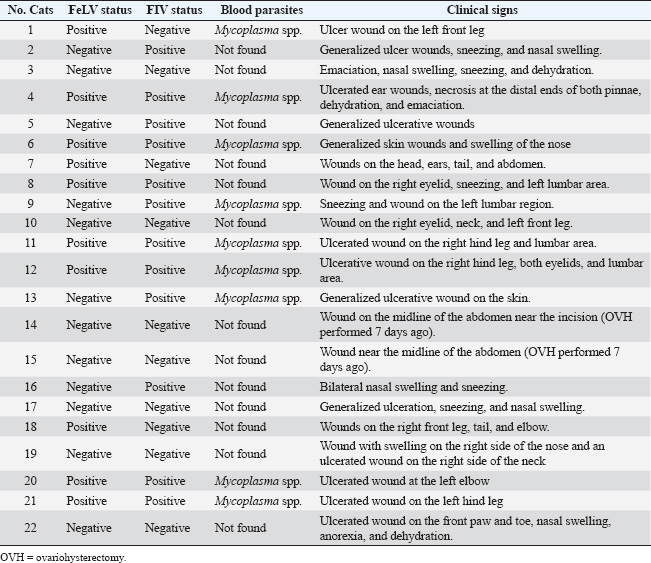
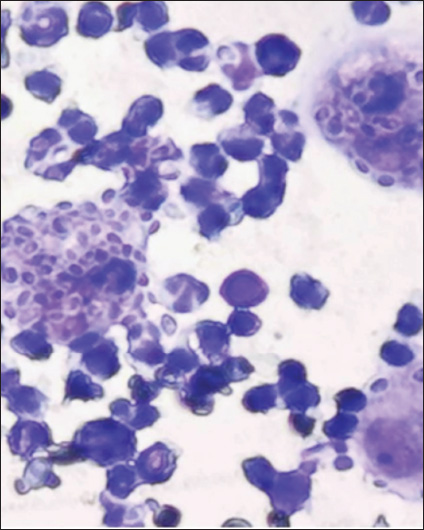
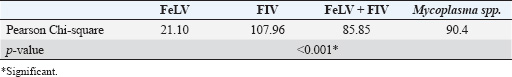
ABSTRACTBackground: Sporotrichosis is a zoonotic fungal infection caused by Sporothrix species and is a growing concern in feline populations due to its potential for transmission to humans. In Thailand, data on the incidence and associated risk factors remain limited, particularly in urban areas such as Bangkok. Aim: To investigate the incidence and potential risk factors of feline sporotrichosis in Thonburi District, Bangkok, Thailand, from 2018 to 2024. Methods: A retrospective review of clinical records was conducted at a veterinary clinic in Thonburi. Among the 1,030 cats examined, 22 cases of sporotrichosis were confirmed through cytological examination. Data collected included sex, neuter status, age, husbandry system, feline leukemia virus (FeLV)/feline immunodeficiency virus (FIV) infection status, and blood parasite infections. Statistical analysis using the chi-square test was performed to identify significant associations between infections and risk factors. Results: The incidence of sporotrichosis was 2.14%. Infected cats were evenly distributed between sexes, with 68.18% being unneutered. All infected cats were domestic shorthairs raised in open systems. Clinical signs included ulcerative skin lesions, sneezing, nasal swelling, anorexia, and dehydration. Co-infection with FeLV, FIV, and Mycoplasma spp. was common. Significant associations were found between sporotrichosis and FeLV, FIV, and Mycoplasma spp. infections (p < 0.001). Follow-up data from five treated cats showed complete recovery within 6 months using itraconazole, with no recurrence after 1 year. Conclusion: Feline sporotrichosis in Thonburi is significantly associated with open husbandry systems and immunosuppressive viral infections. Effective treatment is possible but requires long-term owner compliance. Public education on closed-system cat care and early diagnosis should be included in preventive strategies. These findings support the relevance of the One Health approach in managing zoonotic fungal diseases in urban settings. Keywords: Cat, FeLV, FIV, Mycoplasma spp., Sporotrichosis. IntroductionSporotrichosis is a fungal infection that affects both animals and humans (Rabello et al., 2022). Sporothrix infection is caused by fungi of the genus Sporothrix and can spread through direct contact with open wounds or scratches from infected animals (Alvarez et al., 2022). The fungus is naturally present in the environment, and cats are considered to be the main vectors of this disease (Santos et al., 2024). Infected cats can transmit the disease to other cats through scratches, bites, or wounds on their bodies (Santos et al., 2024). Uncontrolled cat outbreaks can impact animal welfare and lead to legal issues related to animal cruelty (Machado et al., 2021). The incidence of sporotrichosis in cats remains unclear in many countries, although evidence suggests that it is increasing (Santos et al., 2024). Infected cats can spread to stray cat populations, causing difficult-to-control outbreaks and increasing the risk of transmission to humans (Charles-Niño et al., 2022). In medical and epidemiological terms, sporotrichosis is classified as a zoonotic fungal infection that poses a significant public health concern (Charles-Niño et al., 2022). Cat outbreaks can lead to human infection through scratches, bites, or contact with secretions from an infected cat (Silva Neto et al., 2023). If not treated promptly, this can result in a fungal skin infection that may spread to internal organs (Yeow et al., 2023). Diagnosis of feline sporotrichosis is crucial for controlling the spread of infection. The external appearance of lesions in infected cats may resemble other diseases, such as cryptococcosis or bacterial infection (Lin et al., 2023). Therefore, specialized tests, including cytological examination (Makri et al., 2020), culture (Spinelli et al., 2021), or molecular testing (Boechat et al., 2022), are required to confirm the infection. Potential risk factors for infection in cats include open-household systems and latent viral infections that compromise the immune system, such as feline leukemia virus (FeLV) or feline immunodeficiency virus (FIV), which may influence disease severity and transmission potential (Nakasu et al., 2021). Therefore, studying these factors is important for assessing the risk of community transmission and determining appropriate control measures. Materials and MethodsEthical approvalThis study was approved by Suan Sunandha Rajabhat University, Thailand (IACUC 68-001/2025). The secondary data were retrieved from the animal clinic’s records with permission from the owners. Study areaData were collected at an animal clinic located in the Dao Khanong subdistrict, Thonburi district, Bangkok, Thailand (establishment license 01-957/2562; coordinates: 13.707529 latitude, 100.478054 longitude). Study designsThis retrospective study, conducted over a 6-year period from 2018 to 2024, analyzed data from 1,030 cats that visited a veterinary clinic during this time. Cats with Sporothrix infection confirmed by cytological examination The variables recorded for infected cats included age, gender, breed, sterilization status, husbandry system, FeLV-FIV status (tested using the Anigen Rapid FIV Ab/FeLV Ag Test Kit, Korea), and blood smear results for blood parasites (tested at Laboratory of Vet Clinical Center, Bangkok, Thailand). Statistical analysisDescriptive analysis was performed for age, sex, breed, sterilization status, husbandry system, and FeLV/FIV status, with results presented as percentages and mean ± SD. The relationship between the FeLV/FIV status and blood parasite infections with Sporothrix infection was analyzed using the chi-square test. Statistical analysis was conducted using IBM SPSS Statistics, version 29 (IBM Corp., Armonk, NY). ResultsGeneral information on the infected catsA total of 1,030 cats, including 22 infected with Sporothrix, received services at the clinic, representing an incidence rate of 2.14%. Among the infected cats, 11 (50%) were male and 11 (50%) were female. Fifteen of the infected cats (68.18%) were unneutered, whereas seven (31.82%) were neutered. All infected cats were raised in an open system and belonged to the domestic shorthair breed. The average age of the infected cats was 4.41 ± 1.82 years. Table 1 presents details regarding FeLV, FIV, and blood parasite infections. Clinical signs and cytological examinationThe clinical signs in infected cats are nonspecific and include anorexia, dehydration, and ulcerative wounds, which may be generalized on the skin or localized to specific areas such as the eyelids, ears, and tail (Table 1). Additionally, affected cats may exhibit sneezing, nasal wounds, and swelling (Fig. 1). Cytological examination of an impression smear from the lesion, which was stained using the Romanowsky method, revealed yeast capsules. Some yeast cells were observed undergoing phagocytosis, with compacted yeast capsules present within macrophages (Fig. 2). Relationship between FeLV/FIV, blood parasites, and sporotrichosis infection in catsData analysis revealed that 1,008 cats were not infected with Sporothrix during the study period. Among them, 29 cats were infected with FeLV, 16 cats were infected with FIV, 30 cats were coinfected with both FeLV and FIV, and 22 cats were infected with blood parasites. Table 2 presents the analysis of the relationship between FeLV, FIV, and blood parasite infections. DiscussionSporotrichosis has been reported in cats worldwide, including in the United Kingdom (Makri et al., 2020), Brazil (Reis et al., 2024), Chile (Thomson et al., 2023), and Thailand (Chieosilapatham et al., 2023). The disease is caused by a fungal infection commonly found in the environment. Previous reports identified Sporothrix spp., particularly Sporothrix schenckii and Sporothrix brasiliensis, as species of concern due to their potential for transmission in cats (Indoung et al., 2022; de Oliveira et al., 2024). The incidence of feline sporotrichosis in Thailand remains unclear and likely varies according to the outbreak area. The observed incidence in this study was 2.14%. Infected cats were found equally among males and females, which contrasts with the findings of Nakasu et al. (2021), who reported a higher prevalence in male cats. A higher prevalence of sporotrichosis was observed in unneutered cats than in spayed cats, aligning with the findings of Gremião et al. (2021), who noted that sporotrichosis was more common in unneutered males, likely due to behaviors such as fighting, territoriality, and attraction to females. In this study, all infected cats were of the domestic shorthair breed and were raised in an outdoor system. This is consistent with the findings of Nakasu et al. (2021), who reported that all sporotrichosis-infected cats were mixed-breed and kept in outdoor environments, which increased their susceptibility to infection through environmental exposure and fighting. The mean age of infected cats was 4.41 ± 1.82 years, which is consistent with previous reports indicating that sporotrichosis is more common in young cats (Boechat et al., 2022). Table 1. Number of Sporothrix-infected cats, FeLV/FIV status, blood parasites, and clinical signs.
In this study, sporotrichosis in cats was significantly associated with FeLV, FIV, and co-infection with both FeLV and FIV (p < 0.001). However, due to the open husbandry system and the absence of prior testing for FIV and FeLV, determining whether the cats were initially infected with Sporothrix spp. or with the retroviruses is not possible. Previous studies have reported that sporotrichosis-infected cats with high levels of interleukin 10 (IL-10), particularly those coinfected with FIV and FeLV, as well as those with low levels of IL-4 in FeLV-infected cats and IL-12 in FIV-infected cats, tend to exhibit more severe clinical signs (Gremião et al., 2021). The lesions observed in this study were nonspecific and included ulcerative wounds on the legs, skin, and nose. In some cases, infections were found near the midline of the abdomen in cats with a history of ovariohysterectomy (OVH) performed 7 days prior, possibly related to poor postoperative care by the owner. However, lesions resembling those caused by other infections, such as cryptococcosis and histoplasmosis, require careful sampling and differential diagnosis to rule out other possible causes (Barrs et al., 2024). Mycoplasma spp. are blood parasites that infect cats and are typically transmitted via vectors or bite wounds. In this study, infection with Mycoplasma spp. was associated with sporotrichosis. This finding may be related to co-infection with FeLV, FIV, or both. Retroviral infections are commonly found alongside Mycoplasma spp. infections, suggesting that immunosuppression may increase susceptibility to hemotropic mycoplasmas (Carvalho et al., 2024).
Fig. 1. Lesions in cats infected with Sporothrix spp. This image is from the Terdthai Love Pet Clinic. This study used itraconazole at a dose of 30 mg/kg/day (not exceeding 100 mg/day), combined with a liver supplement, and doxycycline at 10 mg/kg/day for 30 days in cases with Mycoplasma spp. infection to treat cats with sporotrichosis (Gremião et al., 2022). Complete follow-up data were available for all five cats. Of these, two tested negative for FIV and FeLV, two were FeLV-positive, and one was FIV-positive. Lesions resolved within 3 months of treatment. Therapy was continued for an additional 3 months, resulting in a total treatment duration of 6 months. A 1-year follow-up revealed no disease recurrence. The recovery time did not differ between cats infected with retroviruses and those not infected. This finding is consistent with that of de Miranda et al. (2018), who reported that the recovery time from sporotrichosis in cats was not associated with retrovirus infection. Treatment outcomes could not be assessed in other cases in the present study because the owners discontinued treatment due to financial constraints. Other drugs reported for the treatment of feline sporotrichosis include potassium iodide (Reis et al., 2024), a combination of itraconazole and potassium iodide (Reis et al., 2024), terbinafine (Viana et al., 2024), and amphotericin B (Gremião et al., 2022). The treatment of cats infected with sporotrichosis requires special care because the disease is slow to cure and can be transmitted to humans. Owner cooperation is essential for successful treatment and recovery. Previous reports have shown that cats whose owners follow veterinary treatment guidelines recover more quickly than those whose owners do not (de Souza et al., 2024). Keeping infected cats in a closed system is also crucial, as it helps prevent the spread of the infection to other cats. Currently, there is no effective vaccine to prevent sporotrichosis (de Almeida et al., 2019). Therefore, preventive care and educating owners about the seriousness of this disease should be prioritized. Future studies should expand the study area, investigate Sporothrix genetic differences in each region, examine other factors affecting virulence and recovery time, and educate cat owners on proper care in accordance with animal welfare standards, including penalties for improper handling.
Fig. 2. Cytological examination using an impression smear at 100× magnification, and cornified epithelial cells, yeast capsules, and clusters of yeast capsules surrounding epithelial cells are observed. Table 2. Relationship between Sporothrix-infected cats and FeLV/FIV status and blood parasite infections.
Study limitationsBecause this study was limited to certain areas of Thailand, including parts of Bangkok, the results may not be representative of the entire country but instead reflect trends in infection risk. The inability to capture some stray cats for treatment is also a limitation of this study. ConclusionThis study identified a 2.14% incidence rate for sporotrichosis in cats in Thonburi, Bangkok. Open husbandry systems and immunosuppression due to FeLV or FIV infection were the primary risk factors associated with infection, with co-infection with Mycoplasma spp. also frequently observed. Statistical analysis revealed a significant association between Sporothrix infection and FeLV, FIV, and Mycoplasma spp. Although itraconazole proved to be effective in treatment, successful outcomes required consistent owner cooperation, with treatment durations often exceeding 3–6 months. Based on the findings, the authors recommend implementing early screening for FeLV, FIV, and Mycoplasma spp. in cats suspected of having sporotrichosis and promoting closed husbandry systems to reduce the risk of infection. Additionally, educating cat owners on the importance of consistent treatment adherence is essential, as successful outcomes often require prolonged therapy lasting more than 3–6 months. AcknowledgementsThe authors would like to thank the Graduate School of Suan Sunandha Rajabhat University, Thailand, for advising on research methods and the Terdthai Love Pet Clinic for providing information. FundingThis research project received no financial support. Authors’ contributionNK defined the research topic, planned data collection, and wrote the manuscript. AL assisted in the design of the experiment, made essential intellectual contributions, and helped draft the manuscript. NP, KT, and NS planned the statistical analysis and contributed to the manuscript. AK and RF also contributed to the manuscript writing and submission. All authors reviewed and approved the final version of the manuscript before submission. Conflict of interestThe authors have no conflicts of interest to declare. Data availabilityAll data supporting this study’s findings are available in the manuscript. ReferencesAlvarez, C.M., Oliveira, M.M.E. and Pires, R.H. 2022. Sporotrichosis: a review of a neglected disease in the last 50 years in Brazil. Microorganisms 10(11), 2152; doi:10.3390/microorganisms10112152 Barrs, V.R., Bęczkowski, P.M., Talbot, J.J., Hobi, S., Teoh, S.N., Hernandez Muguiro, D. and Sandy, J. 2024. Invasive fungal infections and oomycoses in cats: 1. Diagnostic approach. J. Feline Med. Surg. 26(1), 1098612X231219696; doi:10.1177/1098612x231219696 Boechat, J.S., Oliveira, M.M.E., Gremião, I.D.F., Almeida-Paes, R., Machado, A.C.D.S., Zancopé-Oliveira, R.M. and Pereira, S.A. 2022. Sporothrix brasiliensis and feline sporotrichosis in the metropolitan region of Rio de Janeiro, Brazil (1998–2018). J. Fungi 8(7), 749; doi:10.3390/jof8070749 Carvalho, S.F., Pádua, G.T., Paula, W.V.D.F., Tavares, M.A., Neves, L.C., Pereira, B.G. and Krawczak, F.D.S. 2024. Feline vector-borne diseases and their possible association with hematological abnormalities in cats from Midwestern Brazil. Microorganisms 12(11), 2171; doi:10.3390/microorganisms12112171 Charles-Niño, C.L., Loera, A., Medina-Guerrero, E.O., Sanroman-Loza, E.A., Toledo, B. and Pedroza-Roldan, C. 2022. Sporotrichosis: an overview in the context of the one health approach. Curr. Trop. Med. Rep. 9(2), 49–60; doi:10.1007/s40475-022-00250-z Chieosilapatham, P., Chuamanochan, M., Chiewchavit, S., Saikruatep, R., Amornrungsun, E. and Preechasuth, K. 2023. Sporothrix schenckii sensu stricto related to zoonotic transmission in Thailand. Med. Mycol. Case Rep. 41, 44–47; doi:10.1016/j.mmcr.2023.08.003 de Almeida, S.R. 2019. Advances in vaccine development against sporotrichosis. Curr. Trop. Med. Rep. 6, 126–131; doi:10.1007/s40475-019-00183-0 dDe Miranda, L.H.M., Meli, M., Conceição-Silva, F., Novacco, M., Menezes, R.C., Pereira, S.A., Sugiarto, S., Dos Reis, E.G., Gremião, I.D.F. and Hofmann-Lehmann, R. 2018. Co-infection with feline retrovirus is related to changes in immunological parameters of cats with sporotrichosis. PLoS One 13(11), e0207644; doi:10.1371/journal.pone.0207644 dDe Oliveira, P.R.F., De Carvalho, J.A., Costa, T.R., Silva, B.P.E., Da Silva, G.G., Rodrigues, A.M. and Mota, R.A. 2024. Emerging cases of cat-transmitted sporotrichosis driven by Sporothrix brasiliensis in Northeast Brazil. Mycopathologia 189(4), 66; doi:10.1007/s11046-024-00873-y de Souza, B.M., Colombo, S.A., Do Carmo Teixeira, R., Coelho, I.M.P., Barrado, W.D.S., Ramos, B.O.L., Araujo, E.L.M., Bicalho, G.C., De Azevedo, M.I., Keller, K.M., Santos Monti, F.D., Silva Maia, L.D.M., De Magalhães Soares, D.F. and De Oliveira, C.S.F. 2024. Responsible ownership and health education can reduce the time of sporotrichosis treatment in domestic cats. Prev. Vet. Med. 227, 106211; doi:10.1016/j.prevetmed.2024.106211 Gremião, I.D.F., Martins Da Silva Da Rocha, E., Montenegro, H., Carneiro, A.J.B., Xavier, M.O., De Farias, M.R., Monti, F.., Mansho, W.., De Macedo Assunção Pereira, R.H., Pereira, S.A. and Lopes-Bezerra, L.M. 2021. Guideline for the management of feline sporotrichosis caused by Sporothrix brasiliensis and literature revision. Braz.ilian J. Microbiol. 52, 107–124; doi:10.1007/s42770-020-00365-3 Gremião, I.D.F., de Miranda, L.H.M.D., Pereira-Oliveira, G.R., Menezes, R.C., Machado, A.C.D.S., Rodrigues, A.M. and Pereira, S.A. 2022. Advances and challenges in the management of feline sporotrichosis. Rev. Iberoam. Micol. 39(3–4), 61–67; doi:10.1016/j.riam.2022.05.002 Indoung, S., Chanchayanon, B., Chaisut, M., Buapeth, K.O., Morteh, R. and Jantrakajorn, S. 2022. Feline sporotrichosis caused by Sporothrix schenckii sensu stricto in Southern Thailand: phenotypic characterization, molecular identification, and antifungal susceptibility. Med. Mycol. Mycology J. 60(9), myac075; doi:10.1093/mmy/myac075 Lin, E.M., Singer, H., Telang, G.H., Chau, T., Farmakiotis, D. and Robinson-Bostom, L. 2023. Cutaneous Sporothrix globosa infection mimicking cryptococcosis in a patient with history of kidney transplant. J. Cutan. Pathol. 50(7), 629–631; doi:10.1111/cup.14396 Machado, D., Bragança, A., Travnik, I., Rossi, A. and Sant’Anna, A. 2021. Should cats be allowed outdoors? A research survey on animal welfare risks for free-ranging cats in Brazil. Anim. Welfare 30(3), 331–339; doi:10.7120/09627286.30.3.011 Makri, N., Paterson, G.K., Gregge, F., Urquhart, C. and Nuttall, T. 2020. First case report of cutaneous sporotrichosis (Sporothrix species) in a cat in the UK. J. Feline Med. Surg. Open Rep. 6(1), 2055116920906001; doi:10.1177/2055116920906001 Nakasu, C.C.T., Waller, S.B., Ripoll, M.K., Ferreira, M.R.A., Conceição, F.R., Gomes, A.D.R. and Cleff, M.B. 2021. Feline sporotrichosis: a case series of itraconazole-resistant Sporothrix brasiliensis infection. Braz.ilian J. Microbiol. 52, 163–171; doi:10.1007/s42770-020-00290-5 Rabello, V.B.S., Almeida-Silva, F., Scramignon-Costa, B.D.S., Motta, B.D.S., De Macedo, P.M., Teixeira, M.D.M., Almeida-Paes, R.., Irinyi, L.., Meyer, W.. and Zancopé-Oliveira, R.M. 2022. Environmental isolation of Sporothrix brasiliensis in an area with recurrent feline sporotrichosis cases. Front. Cell. Infect. Microbiol. 12, 894297; doi:10.3389/fcimb.2022.894297 Reis, E.G.D., Pereira, S.A., Miranda, L.H.M.D., Oliveira, R.D.V.C.D., Quintana, M.D.S.B., Viana, P.G. and Gremião, I.D.F. 2024. A randomized clinical trial comparing Itraconazole and a combination therapy with Itraconazole and potassium iodide for the treatment of feline Sporotrichosis. J. Fungi 10(2), 101; doi:10.3390/jof10020101 Santos, M.T., Nascimento, L.F.J., Barbosa, A.A.T., Martins, M.P., Tunon, G.I.L., Santos, P.O.M., Dantas-Torres, F. and Dolabella, S.S. 2024. The rising incidence of feline and cat-transmitted sporotrichosis in Latin America. Zoonoses Public Health 71(6), 609–619; doi:10.1111/zph.13169 Silva Neto, F.., Gadelha, C.., Silva, L.., Pazos, N.., Silva, A.., Silva, M.., Sousa, B.., Bernardes Dulgheroff, A.C., Guerra, F.., Magalhães Da Silveira, V.., Oliveira, M.. and Lima Neto, R.. 2023. Case rReport: ocular Sporotrichosis—aA sSeven-cCase sSeries. Am. J. Trop. Med. Hygiene 108(6), 1109–1114; doi:10.4269/ajtmh.22-0501 Spinelli, T.P., Bezerra, L.M., De Souza, B.O.F., Rocha, A., Neto, J.E. and Sá, F.B. 2021. Primary conjunctival sporotrichosis in three cats from Northeastern Brazil. Vet. Ophthalmol. 24(2), 209–215; doi:10.1111/vop.12865 Thomson, P., González, C., Blank, O., Ramírez, V., Río, C.D., Santibáñez, S. and Pena, P. 2023. Sporotrichosis outbreak due to Sporothrix brasiliensis in domestic cats in Magallanes, Chile: a one-health-approach study. J. Fungi 9(2), 226; doi:10.3390/jof9020226 Viana, P.G., Gremião, I.D.F., Da Silva Antonio, I.M., Figueiredo, A.B.F., Correa, M.L., Boechat, J.S., De Sá Machado, A.C., De Oliveira, R.V.C., Oliveira, M.M.E., Almeida‐Paes, R.., Pereira‐Oliveira, G.R. and Pereira, S.A. 2024. Is terbinafine an effective treatment for feline sporotrichosis?. Vet. Rec. 195(4), e4435; doi:10.1002/vetr.4435 Yeow, Y.Y., Tan, X.T. and Low, L.L. 2023. Mucosal sporotrichosis from zoonotic transmission: descriptions of four case reports. Infect. Dis. Rep. 15(1), 102–111; doi:10.3390/idr15010011 | ||
| How to Cite this Article |
| Pubmed Style Kulnides N, Lorsirigool A, Pumipuntu N, Santichat N, Tawinwang K, Kullaya A, Thamyo W, Fongtanakit R. Sporotrichosis incidence and risk factors in cats in Thonburi District, Bangkok, Thailand: A retrospective study. Open Vet. J.. 2025; 15(8): 3677-3683. doi:10.5455/OVJ.2025.v15.i8.31 Web Style Kulnides N, Lorsirigool A, Pumipuntu N, Santichat N, Tawinwang K, Kullaya A, Thamyo W, Fongtanakit R. Sporotrichosis incidence and risk factors in cats in Thonburi District, Bangkok, Thailand: A retrospective study. https://www.openveterinaryjournal.com/?mno=263536 [Access: January 25, 2026]. doi:10.5455/OVJ.2025.v15.i8.31 AMA (American Medical Association) Style Kulnides N, Lorsirigool A, Pumipuntu N, Santichat N, Tawinwang K, Kullaya A, Thamyo W, Fongtanakit R. Sporotrichosis incidence and risk factors in cats in Thonburi District, Bangkok, Thailand: A retrospective study. Open Vet. J.. 2025; 15(8): 3677-3683. doi:10.5455/OVJ.2025.v15.i8.31 Vancouver/ICMJE Style Kulnides N, Lorsirigool A, Pumipuntu N, Santichat N, Tawinwang K, Kullaya A, Thamyo W, Fongtanakit R. Sporotrichosis incidence and risk factors in cats in Thonburi District, Bangkok, Thailand: A retrospective study. Open Vet. J.. (2025), [cited January 25, 2026]; 15(8): 3677-3683. doi:10.5455/OVJ.2025.v15.i8.31 Harvard Style Kulnides, N., Lorsirigool, . A., Pumipuntu, . N., Santichat, . N., Tawinwang, . K., Kullaya, . A., Thamyo, . W. & Fongtanakit, . R. (2025) Sporotrichosis incidence and risk factors in cats in Thonburi District, Bangkok, Thailand: A retrospective study. Open Vet. J., 15 (8), 3677-3683. doi:10.5455/OVJ.2025.v15.i8.31 Turabian Style Kulnides, Narong, Athip Lorsirigool, Natapol Pumipuntu, Nontachai Santichat, Kanokwan Tawinwang, Arunroj Kullaya, Wirongrong Thamyo, and Rachada Fongtanakit. 2025. Sporotrichosis incidence and risk factors in cats in Thonburi District, Bangkok, Thailand: A retrospective study. Open Veterinary Journal, 15 (8), 3677-3683. doi:10.5455/OVJ.2025.v15.i8.31 Chicago Style Kulnides, Narong, Athip Lorsirigool, Natapol Pumipuntu, Nontachai Santichat, Kanokwan Tawinwang, Arunroj Kullaya, Wirongrong Thamyo, and Rachada Fongtanakit. "Sporotrichosis incidence and risk factors in cats in Thonburi District, Bangkok, Thailand: A retrospective study." Open Veterinary Journal 15 (2025), 3677-3683. doi:10.5455/OVJ.2025.v15.i8.31 MLA (The Modern Language Association) Style Kulnides, Narong, Athip Lorsirigool, Natapol Pumipuntu, Nontachai Santichat, Kanokwan Tawinwang, Arunroj Kullaya, Wirongrong Thamyo, and Rachada Fongtanakit. "Sporotrichosis incidence and risk factors in cats in Thonburi District, Bangkok, Thailand: A retrospective study." Open Veterinary Journal 15.8 (2025), 3677-3683. Print. doi:10.5455/OVJ.2025.v15.i8.31 APA (American Psychological Association) Style Kulnides, N., Lorsirigool, . A., Pumipuntu, . N., Santichat, . N., Tawinwang, . K., Kullaya, . A., Thamyo, . W. & Fongtanakit, . R. (2025) Sporotrichosis incidence and risk factors in cats in Thonburi District, Bangkok, Thailand: A retrospective study. Open Veterinary Journal, 15 (8), 3677-3683. doi:10.5455/OVJ.2025.v15.i8.31 |