| Research Article | ||
Open Vet. J.. 2025; 15(9): 4592-4600 Open Veterinary Journal, (2025), Vol. 15(9): 4592-4600 Research Article Possible involvement of cerebrospinal fluid drop metastasis in the survival of French bulldogs after radiotherapy for presumed glial brain tumorsMunekazu Nakaichi1*, Yuki Nemoto1, Toshie Iseri2, Harumichi Itoh3, Hiroshi Sunahara4, Takuya Itamoto4, Kazuhito Itamoto3 and Kenji Tani41Department of Veterinary Radiology, Joint Faculty of Veterinary Science, Yamaguchi University, Yamaguchi, Yamaguchi 753-8515, Japan 2Department of Cooperative Department of Veterinary Medicine, Animal Medical Emergency Center, Tokyo University of Agriculture and Technology, Kokanei, Tokyo, 184-8588, Japan 3Department of Veterinary Small Animal Clinical Science, Joint Faculty of Veterinary Science, Yamaguchi University, Yamaguchi, Yamaguchi 753-8515, Japan 4Department of Veterinary Surgery, Joint Faculty of Veterinary Science, Yamaguchi University, Yamaguchi, Yamaguchi 753-8515, Japan *Corresponding Author: Munekazu Nakaichi. Department of Veterinary Radiology, Joint Faculty of Veterinary Science, Yamaguchi University, Yamaguchi, Yamaguchi 753-8515, Japan. Email: nakaichi [at] yamaguchi-u.ac.jp Submitted: 17/04/2025 Revised: 29/07/2025 Accepted: 18/08/2025 Published: 30/09/2025 © 2025 Open Veterinary Journal
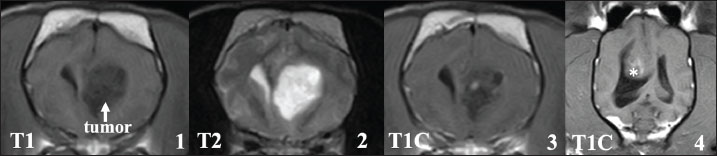
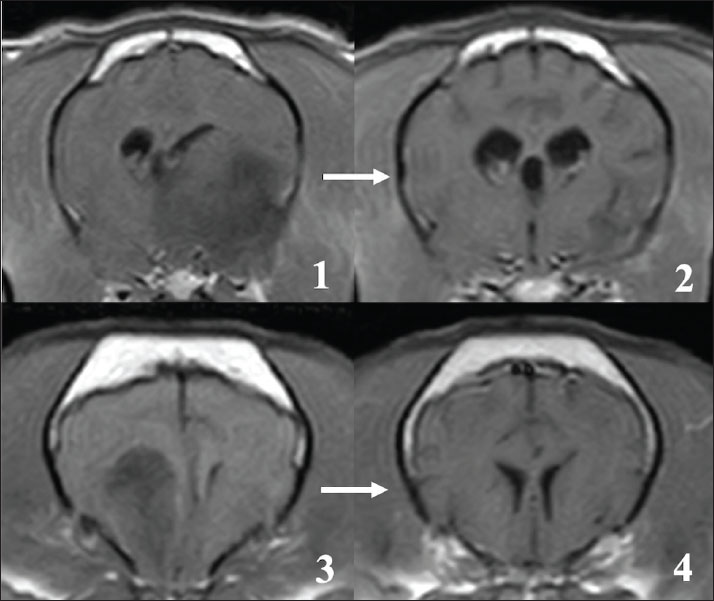
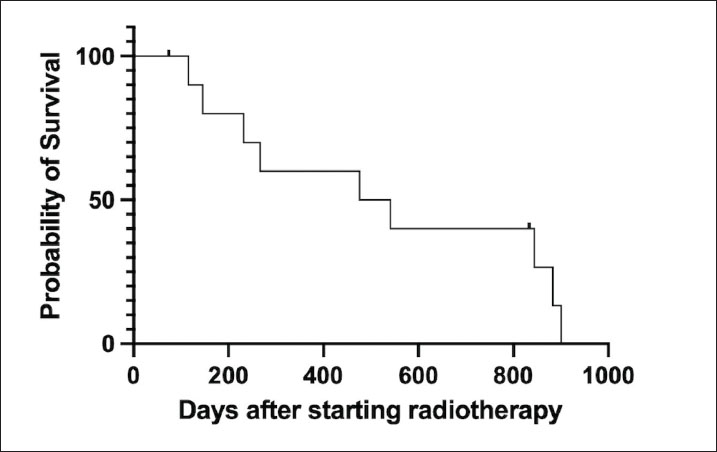
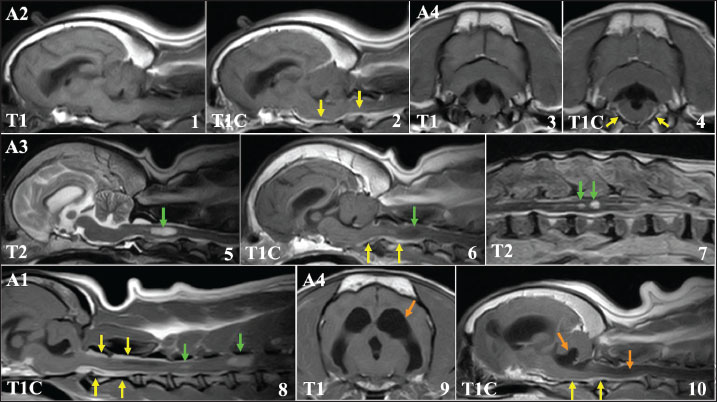
AbstractBackground: The French bulldog (FB) is a popular breed, and the number of FBs raised has increased. In recent years, there has been an increasing number of reports of FB brain tumors. Radiotherapy is widely used and believed to be the most effective therapeutic modality against brain tumors in small animal clinical practice; therefore, it is necessary to examine the outcomes of radiation therapy for brain tumors of FB. Aim: This study aimed to investigate the therapeutic effectiveness of radiotherapy on presumed glial brain tumors in FBs and to investigate the possible causes of poor prognosis of patients by reviewing magnetic resonance imaging (MRI) findings at clinical worsening after radiotherapy. Methods: Medical records and MRI images of 15 FBs with presumed glial tumor based on MRI that were treated by radiotherapy were retrospectively analyzed. Results: Among the 15 FB cases, 11 completed their originally scheduled radiotherapy. Radiotherapy reduced the size of primary tumors on MRI in 11 cases; however, the median survival time (MST) of these 11 cases was 509 (range: 74–900), which contrasts with previous reports of radiotherapy for canine brain tumors. The major cause of death was the recurrence of neurological symptoms. MRI features of recurrent cases and cases that died in the early clinical course were characterized by clear enhancement in the leptomeningeal region around the brainstem to the cervical spinal cord, although primary lesions remained. These MRI findings were compatible with those of CSF drop metastasis. Conclusion: Our findings reveal that the primary lesions in FB glial brain tumors are radiosensitive. However, CSF drop metastasis might account for the recurrence of clinical symptoms and shorten the survival time in the affected FBs, and CSF drop metastasis should be considered, even after tumor regression. Keywords: Brain tumor, CSF drop metastasis, Dog, French Bulldog, Radiotherapy. IntroductionBecause of advances in diagnostic imaging technology in the veterinary field, canine brain tumors are more often diagnosed or treated because we have better equipment, and owners are more willing to perform diagnostic work-up and treatment nowadays. The number of clinical reports on canine brain tumors has recently increased, furthering our clinical understanding of these entities (Miller et al., 2019; José-López et al., 2021; Rossmeisl & Pancotto, 2020). Meningioma is the most common histopathological tumor type in dogs (Kishimoto et al., 2020; Snyder et al., 2006; Song et al., 2013; Van Asselt et al., 2020; Schwarz et al., 2018). In addition to meningiomas, various histopathological types, including glial tumors such as astrocytoma and oligodendroglioma, choroid plexus tumors, and pituitary tumors, have been investigated for their clinical features and treatment outcomes (Miller et al., 2019; Rossmeisl & Pancotto, 2020). To date, megavoltage radiotherapy has been considered the most effective treatment modality for canine brain tumors (Debreuque et al., 2020; MagalhÃes et al., 2021; Dolera et al., 2018; Schwarz et al., 2018; Treggiari et al., 2017; Van Asselt et al., 2020). Brain tumors in the French bulldog (FB) have recently been reported (Hasegawa et al., 2012; Kishimoto et al., 2020; Mayousse et al., 2017; Nakamoto et al., 2018). One epidemiological study in Japan suggested that the FB is a breed that is predisposed to brain tumors. Furthermore, the histopathological features of FB tumors suggest that they are predominantly oligodendrogliomas derived from one of the glial cell lineages (Kishimoto et al., 2020). As surgical resection of glial tumors in dogs is technically difficult because of their location and the risk to surrounding normal brain tissue (Forward et al., 2022), radiation therapy may be a more suitable treatment modality for FB brain tumors. During 2017–2022, we treated 15 cases of glial tumors in FBs with definitive-intent radiotherapy in our veterinary hospital. Good clinical outcomes were obtained for the primary lesions; however, cerebrospinal fluid drop metastasis of the tumor cells, which was recently reported in canine brain tumors, may have shortened the survival time of the brain tumor cases (Bentley et al., 2021; Vigeral et al., 2018). This study aimed to investigate the therapeutic effectiveness of radiotherapy on presumed glial brain tumors in FBs. The possible involvement of CSF drop metastasis in the survival of these brain tumor cases after radiotherapy was also discussed based on the survival data and MRI features of the affected FBs. Materials and MethodsCasesThis study included 15 cases of presumed grail tumor in FBs that were referred to our veterinary hospital between 2017 and 2022. The characteristics of these cases on MRI strongly suggested that they were derived from glial cells, and based on previous reports, they were considered highly likely to be oligodendroglioma (Hasegawa et al., 2012; Kishimoto et al., 2020; Mayousse et al., 2017; Nakamoto et al., 2018). In one case, image-guided biopsy was performed via a small borehole in the skull, resulting in a histopathological diagnosis of oligodendroglioma. There were 9 other cases of FB brain tumors during the study period; however, these cases were excluded from the study because their MRI features suggested a histopathological type other than glial tumor (5 cases of meningioma and 2 cases each of pituitary tumor and choroid plexus tumor). These patients visited our hospital for MRI examination to check for neurological abnormalities and were treated with megavoltage radiotherapy. All patients were subjected to permanent-type MRI examination under general anesthesia and diagnosed with brain tumors. A permanent-type MRI unit was used in this study (0.4tesla, APERTO InspireTM, Hitachi Medico, Tokyo, Japan). All dogs were placed in the gantry in a prone position, and a surface coil for the human stifle joint was used for MRI. Fast spin echo (FSE) sequence was used in all patients, and T1- (TR=360 ms, TE=13 ms) and T2-weighted (TR=5000 ms, TE=100 ms) images were obtained in transverse, sagittal, and coronal directions. The slice width was 4 mm without interslice gaps. After the acquisition of T1- and T2-weighted images, a contrast-enhanced study was performed using intravenous administration of gadoteridol (0.2 ml/kg, iv. ProHanceTM, Eisai Co., Ltd., Tokyo). The MR images of the tumors were examined for their location, relation to ventricles, number of tumor tissues, signal intensity in T1- and T2-weighted images, and enhancing effect of contrast media. RadiotherapyAll owners of the 15 FB patients requested definitive-intent radiotherapy using a linear accelerator (Elekta Synergy PlatformTM, Elekta, Stockholm, Sweden) with a multileaf-collimator with 5-mm leaves. To prepare treatment plans, a planning CT scan was performed on each dog before treatment using a 64 multi-slice CT scanner (SupriaTM, Hitachi Medico, Tokyo, Japan). All dogs were positioned in a sternal recumbent position, which was immobilized with a vacuum cushion and a resin maxillary dental profile. In all patients, 1.25-mm slice thickness CT image datasets were obtained with or without an intravenous contrast medium of iopamidol (1.5 ml/kg, i.v., Iopamidol 370 FTM, Fuji Pharma Co., Ltd. Toyama, Japan), which were used for treatment planning. Treatment plans were developed using a planning system (Monaco version 5.51TM, Elekta, Stockholm, Sweden). Gross tumor volume (GTV) contoured on 1.25-mm CT images. Fusion MRI and CT images were used to contour the GTV in all cases. The clinical target volume (CTV) was delineated to include 2 mm around the GTV, and the planning target volume (PTV) was defined with a margin of 2 mm around the CTV. The irradiation protocol comprised intensity-modulated radiation therapy (IMRT) using 4 or 6 MV beams. The treatment planning goal was to deliver 100% of the dose to 95% of the PTV. A total dose of 42 Gy divided into 10 fractions was planned for all cases; 4.2 Gy was given twice a week for 10 doses over 5 weeks. Before each daily treatment, image guidance for patient positioning accuracy with on-board MV radiography (iView GTTM, Elekta, Stockholm, Sweden) in two orthogonal directions was performed, and positional errors were corrected. Radiation therapy was performed under general anesthesia and adequate anesthesia management. All patients were anesthetized by intravenous administration of propofol (Propofol Intravenous Injection MaruishiTM, Maruishi Pharmaceutical Co., Ltd., Osaka, Japan) or alfaxalone (to effect, AlfaxanTM, Jurox Pty Limited, New South Wales, Australia), and after tracheal intubation, anesthesia was maintained by inhalation anesthesia with sevoflurane (MylanTM, Mylan Pharmaceutical Co., Ltd., Tokyo, Japan). Intravenous administration of D-mannitol (1 g/kg, dripping for 30 min, 15% Mannitol InjectionTM, Terumo, Tokyo, Japan) was administered to all patients as treatment for elevated intracranial pressure prior to anesthesia induction. Follow-up of casesMRI was examined immediately after the 5th and last radiotherapy fraction. During the follow-up period after radiotherapy, clinical signs were observed by the patients’ owners, and follow-up MRI was scheduled at regular follow-up examinations in all cases. In addition, an MRI was performed in four cases (cases A1–A4) when the clinical signs worsened because of possible tumor progression. In cases of clinical recurrence, symptomatic treatment with corticosteroids and antiepileptics was performed as needed. In the other 4 cases that could not complete radiotherapy due to early death in the treatment course (cases B1–B4), MR images at the first and 5th visit were re-checked to identify factors contributing to their poor prognosis. The overall survival time of the cases with radiotherapy, defined as the duration from the start of radiation therapy to the date of death, was determined for 14 cases based on medical records or telephone interviews with referring veterinarians, dog owners, or both. The median survival time (MST) and Kaplan–Myeier curve of the patient group were obtained using a commercially available software (Prism version 9.3.1, GraphPad Software, San Diego, CA, USA). Ethical approvalNot needed for this study. ResultsBackground and clinical characteristics of the casesThe 15 cases comprised one male, five castrated males, three females, and six spayed females, and the average age of the dogs was 8.4 years (range, 4.4–14.6 years). Seizures (80.0%), ataxia (33.3%), compulsive walking (20.0%), and head tilting (6.7%) were the main clinical symptoms that resulted in the visits. Two patients had severely elevated intracranial pressure on MRI and were unable to stand at the time of initial examination. One patient had severe brachycephalic obstructive airway syndrome that required surgical correction. Magnetic resonance imaging of presumed glial tumors Brain tumors in all 15 cases were present in the cerebrum and were suspected to be tumors derived from glial cells (Fig. 1). Among the 15 cases, 14 cases had a single tumor site, and one case had 2 tumor sites in the cerebrum on MRI. Furthermore, 11 of the 15 cases appeared to be in contact with the lateral ventricles, and in 3 cases, the tumor tissues seemed to invade into the lateral ventricles on MRI. Although the signal intensity on MRI of these glial tumors varied, most cases showed low to iso-signal intensity on T1-weighted images and iso- to high-signal intensity on T2-weighted images. The enhancing effect of the contrast medium also varied among the cases; one case showed a clear ring-enhancing effect, 2 cases showed homogenous enhancement (one case with a ring-shaped periphery), and 7 cases showed heterogenous enhancement (three cases with a ring-shaped periphery). The remaining 5 cases showed almost no enhancement. Cerebellar herniation, possibly induced by the intracranial tumor, was observed in two cases. Additional CT evaluations of the thoracic and abdominal cavities at the first visit showed no distant metastatic lesions and other abnormal findings in any of the patients. RadiotherapyOne patient died during treatment planning and could not receive radiotherapy (B1). The cause of death was unknown. The other 3 cases died in the radiation therapy course because of worsening clinical symptoms during the treatment course; 2 and 1 cases died after the first and 8th fraction of the radiotherapy, respectively (B2-4). The remaining 11 patients completed their originally scheduled radiotherapy. Radiotherapy improved the clinical symptoms of all patients who completed treatment, completing the radiotherapy schedule. In 7 cases with persistent seizure, antiepileptic medication was continued during and after radiotherapy. However, locomotor dysfunctions, such as ataxia and compulsive walking, improved in all 11 cases. MRI examinations performed after the final dose showed regression of primary tumor tissues in all cases (Fig. 2). In 7 cases, tumor tissue completely disappeared on MRI, and in the other 4 cases, showed apparent reductions and in tumor size as measured on MRI images. In all cases, CT evaluations of the thoracic and abdominal cavities performed with the last dose of the radiotherapy showed no distant metastatic lesions. At the end of radiotherapy, all patients were in an acceptable physical condition. However, in 4 cases, the neurological signs recurred after a period of clinical stability, and the owners of these cases requested MRI re-evaluation when clinical symptoms recurred (cases A1–A4). The median duration between the end of radiotherapy and clinical worsening was 256 (range: 28-457) days. At the time of recurrence, all 4 cases exhibited ataxia, and 1 case could not stand unaided. In addition, epileptic seizures recurred in 2 of the 4 cases despite antiepileptic medical treatment. The MRI features of these cases are described in detail below. These cases then worsened, with death eventually resulting from the progression of neurological symptoms. At the time of writing, 12 of the 14 cases died, and at least 11 might have died from tumor progression based on the condition at the time of visit and/or interviews with dog owners. The median survival time of 14 patients who started radiotherapy and 11 patients who completed radiotherapy were 267 (range: 1–900) and 509 (74–900) days, respectively (Fig. 3). Magnetic resonance imaging of recurrent cases (A1–A4)The MRI features of these recurring cases (A1–A4) are shown in Fig. 4. In all 4 cases, MRI showed that the primary tumor tissues had almost completely disappeared. However, in the contrast study, sagittal T1-weighted images of these 4 cases showed clear enhancement in the leptomeningeal region, which was most evident in the area spanning the ventral side of the brainstem to the cervical spinal cord (Fig.4,1-4). In addition to these leptomeningeal enhancements, two cases (A1 and A3) had space-occupying lesions in the cervical and/or thoracolumbar spinal cord along the central canal of the spinal cord (Fig.4,5-8). The signal intensities of both lesions were slightly low in T1-weighted images, and slightly high in T1-weighted and T2-weighted images, respectively. The spinal lesion showed only minor enhancement in one patient, but there was clear enhancement in the other. Furthermore, in case A3, multiple mass lesions were found in the thoracolumbar spinal cord (Figs. 4 and 7). Significant obstructive hydrocephalus was observed in one case (A4, Fig.4, 9-10). These findings are highly similar to those showing CSF drop metastasis, which was recently reported in dogs (Vigeral et al., 2018; Bentley et al., 2021).
Fig. 1. Typical MRI findings of the presumed glial tumors observed in this study. In many cases, brain tumors showed low signal intensity on T1-weighted images (1) and high signal intensity on T2-weighted images (2). Various enhancing effects were observed in the contrast examination, but most of them showed relatively weak enhancement (3). Some tumor tissues that clearly protruded into the ventricles were also observed (4, asterisk).
Fig. 2. The effect of radiotherapy on primary brain tumors in FBs. 1, 3: MRI findings before irradiation (contrast-enhanced T1-weighted image). 2, 4: MRI findings immediately after the final fraction of radiotherapy (contrast-enhanced T1-weighted image). Tumor tissue almost disappeared on MRI after radiotherapy.
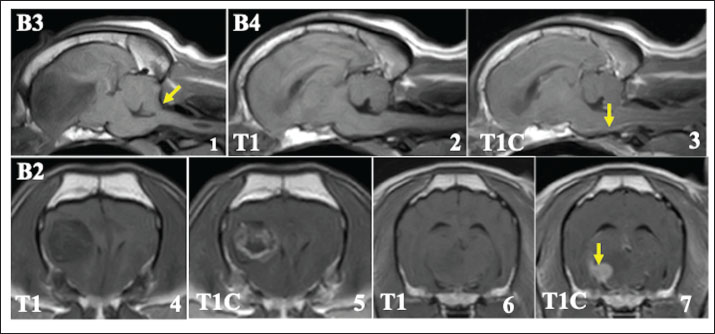
Fig. 3. Kaplan–Meier survival curve of 11 FB cases of presumed glial tumors with radiotherapy completion. The median survival time was 509 days (range, 74–900 days). The clinical symptoms of these 4 cases with presumed CSF drop metastasis (A1-A4) gradually worsened despite corticosteroid and antiepileptic treatments, and these dogs ultimately died of disease progression. The median duration from recurrence to death of the 4 cases (A1-A4) was 51 days (range: 9–106 days). Magnetic resonance imaging of four early deaths (B1–B4)In this study, 4 cases could not complete the radiation therapy. Among these, 1 case died before starting treatment (B1), and 3 cases died during radiation therapy (B2–B4). Although the cause of death was not clearly identified because an autopsy could not be done, 2 cases that died after the first fraction showed cerebellar herniation on MRI at the first visit, possibly due to large tumor size (Fig. 5,1). On MRI at the first admission in these 4 cases, leptomeningeal enhancement, as seen in cases A1–A4, was also observed, although the changes were less prominent (Fig. 5, 1-3). In 1 case (B2), multiple mass lesions were observed. In addition to the primary lesion, another presumed tumor tissue was observed, which appeared to be contiguous with the meninges on MRI, showing clear enhancement (Fig.5, 4-7). DiscussionBrain tumors are the most common neurological diseases that cause encephalopathy in FB (Mayousse et al., 2017), and some recent clinical cases of FB brain tumor have been described (Hasegawa et al., 2012; Nakamoto et al., 2018269). In 2006, a large-scale epidemiological report of canine brain tumors in 2006 did not include any FB cases (Snyder et al., 2006). However, a 2013 report included a few FB cases (Song et al., 2013), and a more recent report in 2021 in Japan reported that FBs were predisposed to brain tumors, especially oligodendroglioma (Kishimoto et al., 2020). The cause of the rise in FB brain tumor cases remains unclear; the increase in the number of FBs raised, both domestically and abroad, is likely an important contributing factor (O’Neill et al., 2018). In addition, because genetic abnormalities are involved in the development of some neoplastic diseases, poorly-planned breeding to meet the increasing demand for FBs as companion animals may have contributed to the rapid increase in brain tumors. Furthermore, mating to maintain particular physical features might also be a factor contributing to the increasing number of brain tumors in FBs as reported in other disorders (O’Neill et al., 2018; O’Neill et al., 2021).
Fig. 4. MRI findings of FB cases in which clinical symptoms recurred after radiotherapy (cases A1–A4, T1: T1-weighted image, T2: T2-weighted image, T1C: T1-weighted image with contrast medium). Upper lane (1–4): A clear enhancement was observed in the meninges around the brainstem (yellow arrows). Middle lane (5–7): Spinal lesions observed at clinical recurrence (green arrows). The lesion located in the central cervical spinal cord of case A3 showing high-signal intensity on T2-weighted image (5) showed no contrast enhancement (6, green arrow), whereas the leptomeningeal region showed clear enhancement (6, yellow arrows). Multiple lesions were also observed in the thoracolumbar spinal cord in this case (7). Lower lane (8–10): Cervical spinal lesions in patient A1. Unlike case A3, these lesions showed clear enhancement, similar to that of the leptomeningeal region (8, green arrows). In case A4, severe obstructive hydrocephalus was observed, with dilated lateral (9) and fourth (10) ventricles (orange arrows). FB brain tumors are predominantly of glial origin, with a predominance of oligodendrogliomas (Kishimoto et al., 2020). In this study, only one case was histopathologically confirmed as oligodendroglioma, but the MRI characteristics of the presumed grail tumors of the FB included in this series were quite similar to those of canine oligodendroglioma reported previously (Hasegawa et al., 2012; Miller et al., 2019; Nakamoto et al., 2018; Rossmeisl & Pancotto, 2020). Therefore, although not definitive, most of the cases described here were probably oligodendrogliomas. Radiotherapy for FB oligodendrogliomas has been reported, showing that FB glial tumors might be radiosensitive (Hasegawa et al., 2012; Nakamoto et al., 2018). In our study, the size of the brain tumors also markedly decreased on MRI after radiotherapy, and clinical symptoms improved in almost all cases. Although the number of cases in this study was quite limited, our findings suggest that radiotherapy might be effective in treating glial tumors in FBs, as previously reported. However, the mean MST after completion of radiotherapy was 509 days, despite good management of the primary lesions, as confirmed by MRI after radiotherapy. The latest reports on radiotherapy outcomes for canine brain tumors from various institutions have shown superior MSTs of 500–1000 days (Debreuque et al., 2020; MagalhÃes et al., 2021; Monforte Monteiro et al., 2020; Van Asselt et al., 2020). Therefore, the mean MST in our present study is comparatively short. These results suggested that the prognosis of FB glial tumors remained guarded despite the good response of the primary lesions to radiotherapy. Therefore, some other problems may be underlying the shorter MST.
Fig. 5. MRI at the first visit of the cases that died early after visiting our hospital (cases B2–B4, T1: T1-weighted image, T2: T2-weighted image, and T1C: T1-weighted image with contrast medium). Upper lane 1: Cerebellar herniation was observed on the sagittal plane (yellow arrow) in case B3, possibly due to the large tumor size. Upper lanes 2 and 3: At the time of the first visit, enhancement was already observed in the leptomeningeal region around the brainstem (B4, yellow arrow), but was less prominent compared with cases A1–A4. Lower lane 4–7: In case B2, the tumor tissue considered to be the primary lesion showed heterogeneous enhancement (4, 5). Furthermore, another mass contiguous with the meninges was observed. This mass shows a clear enhancement (6, 7, yellow arrow). To investigate the causes of the shorter MST, we re-examined the MR images obtained at the recurrent phase in four cases (A1–A4). Contrast enhancement of the leptomeninges around the brainstem was observed in all 4 cases. In a report by Vigeral et al. (2018), similar MRI findings of ventral brainstem leptomeningeal enhancement were obtained after radiotherapy for oligodendroglioma in the English bulldog, and the investigators interpreted these data as indicative of CSF drop metastasis, using this term for the first time in small animal practice. CSF drop metastasis refers to tumor metastatic forms in which metastatic lesions are formed within the brain, and in some cases, within and/or around the spinal cord by tumor cells disseminated into the CSF. Nakamoto et al. (2018) reported similar MRI findings, suggestive of CSF drop metastasis, during follow-up of an oligodendroglioma in a single case of FB treated with radiotherapy. In the report, acceptable local control of the primary lesion was obtained before clinical symptom recurrence, as in our cases. In addition to leptomeningeal enhancement around the brainstem, lesions in the spinal cord and an obstructive hydrocephalus were concurrently observed at the recurrent phase in 2 cases and in one case, respectively. These MRI features have also been described in previous reports; in their cases, Vigeral et al. (2018) and Nakamoto et al. (2018) reported lesions in the spinal cord and significant hydrocephalus, respectively. The MRI findings in the present study were consistent with previously reported characteristics of CSF drop metastasis. Furthermore, in the other 4 cases that died early in their treatment course (B1–B4), the characteristics of CSF drop metastasis might have been present on MRI at the first visit, although less prominently. In these cases, it is possible that CSF drop metastases had already occurred at the time of the first visit, and they might have resulted in more severe clinical symptoms compared with those cases with completed radiotherapy. In case B2, a tumor lesion other than the primary tumor that was contiguous with the meninges was observed. These meningeal mass lesions are similar to those in the MR images showing CSF drop metastasis in a previous report (Bentley et al., 2021). The effect of CSF drop metastasis on survival time in FB with oligodendroglioma could not be accurately determined because the definitive cause of death in most cases could not be identified in this study. However, given that the MST of the FBs in this study did not sufficiently prolong, CSF drop metastasis may shorten the survival of FB glial tumor cases. The mechanism by which CSF drop metastasis occurs remains unclear; however, several hypotheses have been proposed. The close positional relationship between brain tumors and the ventricular system is an important cause of CSF drop metastasis. Bley et al. (2021) examined the relationship between tumor location in the cerebrum and prognosis. Brain tumors close to the subventricular zone (SVZ), defined as the region just under the ependymal cells of the base of the lateral ventricle, were associated with a poorer prognosis and a shorter MST. The close proximity of the brain tumor to the ventricles might easily disrupt the ependymal cells, facilitating their spread into the ventricles. In our current study, tumors appeared to be located in the SVZ in 11 of the 15 cases, and 3 cases had apparently protruding tumor tissue in the ventricles on MRI. Our results are consistent with Rohrer Bley’s finding of poor prognosis of brain tumors involving the SVZ (Rohrer Bley et al., 2021). Few studies have been conducted on the treatment of canine CSF drop metastasis. One of the reasons for the short MST in the present study may be the lack of additional treatment for CSF drop metastasis after radiation therapy, other than symptomatic treatment. Theoretically, the use of chemotherapeutic agents that are easily distributed in the CSF is the most effective treatment for CSF drop metastasis. Lomustine is currently used for CNS tumors in dogs. Hasegawa et al. (2012) used lomustine to treat oligodendroglioma in an FB in which CSF drop metastasis was suspected after radiotherapy, resulting in a longer survival period of 910 days, although the term CSF drop metastasis was not used in that report. Therefore, lomustine may have therapeutic potential for CSF drop metastasis. Recently, temozolomide has also been investigated for the treatment of canine brain tumors (Dolera et al., 2018; Hicks et al., 2019; Tonogai et al., 2021), but its efficacy remains unclear because of limited clinical data. Another possible treatment is extensive radiation, including the whole brain and spinal cord. However, no such treatment has been reported in the veterinary field. Because CSF drop metastases are probably life-threatening, further studies are warranted to prolong the survival of dogs with brain tumor and CSF drop metastasis. There are several limitations to this study. In this study, a permanent-type MRI was used; however, due to its imaging performance, it may have been difficult to accurately judge the details of the MRI findings. Using a superconducting-type MRI would have been preferable. In addition, histopathological examination of the brain tumors was not performed except for one case. These cases likely had oligodendroglioma based on previous reports, but additional histopathological studies might be needed. In addition, because no autopsy was performed in this study, the detailed cause of death remained unknown. In our cases, diagnostic imaging strongly suggested the occurrence of CSF drop metastases associated with brain tumors, but autopsy is needed to provide clear evidence of these CSF drop metastases and their association with death. Furthermore, because this is a small study conducted at a single facility, our findings should be corroborated and extended by larger-scale multicenter studies. ConclusionThis study demonstrated that primary lesions in FB glial brain tumors were considered radiosensitive. However, CSF drop metastasis might account for the recurrence of clinical symptoms and shorten the survival time in patients with FBs. Based on these findings, CSF drop metastasis in some types of canine brain tumors should be given attention, even after tumor regression. AcknowledgementsWe thank Barry Patel, PhD, from Edanz (https://jp.edanz.com/ac), for editing a draft of this manuscript. FundingThe author received no financial support for the research and/or publication of this article. Authors’ ContributionsDiagnostic imaging at the first visit and follow-up examination were performed by Munekazu Nakaichi, Yuki Nemoto, and Toshie Iseri. Yuki Nemoto and Toshie Iseri planned and performed radiotherapy. Harumichi Ito, Hiroshi Sunahara, and Takuya Itamoto performed anesthesia management during MRI examinations and radiotherapy. Munekzu Nakaichi, Kenji Tani, and Kazuhito Itamoto wrote the first draft, and all authors read and approved the final draft. Conflict of interestThe author declares no potential conflicts of interest with respect to this article’s research, authorship, and/or publication. Data availabilityAll data supporting this study’s findings are available within the manuscript. ReferencesBentley, R. T., Yanke, A. B., Miller, M. A., Heng, H. G., Cohen-Gadol, A. and Rossmeisl, J. H. 2021. Cerebrospinal Fluid Drop Metastases of Canine Glioma: Magnetic Resonance Imaging Classification. Front. Vet. Sci. 8, 650320. Debreuque, M., De Fornel, P., David, I., Delisle, F., Ducerveau, M. N., Devauchelle, P. and Thibaud, J. L. 2020. Definitive-intent uniform megavoltage fractioned radiotherapy protocol for presumed canine intracranial gliomas: retrospective analysis of survival and prognostic factors in 38 cases (2013-2019). BMC Vet. Res. 16, 412. Dolera, M., Malfassi, L., Bianchi, C., Carrara, N., Finesso, S., Marcarini, S., Mazza, G., Pavesi, S., Sala, M. and Urso, G. 2018. Frameless stereotactic radiotherapy alone and combined with temozolomide for presumed canine gliomas. Vet. Comp. Oncol. 16, 90-101. Forward, A. K., Volk, H. A., Cherubini, G. B., Harcourt-Brown, T., Plessas, I. N., Garosi, L. and De Decker, S. 2022. Clinical presentation, diagnostic findings and outcome of dogs undergoing surgical resection for intracranial meningioma: 101 dogs. BMC Vet. Res. 18, 88. Hasegawa, D., Uchida, K., Kuwabara, T., Mizoguchi, S., Yayoshi, N. and Fujita, M. 2012. Long-term survival in a dog with anaplastic oligodendroglioma treated with radiation therapy and CCNU. J. Vet. Med. Sci,.74, 1517-1521. Hicks, J., Platt, S., Stewart, G., Senneca, C., Holmes, S., Kent, M., Howerth, E., Kaplan, J. and Kaplan, E. 2019. Intratumoral temozolomide in spontaneous canine gliomas: feasibility of a novel therapy using implanted microcylinders. Vet. Med. Sci. 5, 5-18. José-López, R., Gutierrez-Quintana, R., de la Fuente, C., Manzanilla, E. G., Suñol, A., Pi Castro, D., Añor, S., Sánchez-Masian, D., Fernández-Flores, F., Ricci, E., Marioni-Henry, K., Mascort, J., Matiasek, L.A., Matiasek, K., Brennan, P.M. and Pumarol, M. 2021. Clinical features, diagnosis, and survival analysis of dogs with glioma. J. Vet. Intern. Med. 35, 1901-1917. Kishimoto, T. E., Uchida, K., Chambers, J. K., Kok, M. K., Son, N. V., Shiga, T., Hirabayashi, M., Ushio, N. and Nakayama, H. 2020. A retrospective survey on canine intracranial tumors between 2007 and 2017. J. Vet. Med. Sci. 82, 77-83. MagalhÃes, T. R., BenoÎt, J., NÉČovÁ, S., North, S. and Queiroga, F. L. 2021. Outcome After Radiation Therapy in Canine Intracranial Meningiomas or Gliomas. In Vivo 35, 1117-1123. Mayousse, V., Desquilbet, L., Jeandel, A. and Blot, S. 2017. Prevalence of neurological disorders in French bulldog: a retrospective study of 343 cases (2002-2016). BMC Vet. Res. 13, 212. Miller, A. D., Miller, C. R. and Rossmeisl, J. H. 2019. Canine Primary Intracranial Cancer: A Clinicopathologic and Comparative Review of Glioma, Meningioma, and Choroid Plexus Tumors. Front. Oncol. 9, 1151. Monforte Monteiro, S. R., Rossmeisl, J. H., Russell, J., Holmes, M. A., Wessmann, A., Morris, J., Dobson, J.M. and Vanhaesebrouck, A. E. (2020). Effect of radiotherapy on freedom from seizures in dogs with brain tumors. J. Vet. Intern. Med. 34, 821-827. Nakamoto, Y., Fukunaga, D., Uchida, K., Mori, T., Kishimoto, T. and Ozawa, T. 2018. Anaplastic oligodendroglioma with leptomeningeal dissemination in a french bulldog. J. Vet. Med. Sci. 80, 1590-1595. O’Neill, D. G., Baral, L., Church, D. B., Brodbelt, D. C. and Packer, R. M. A. 2018. Demography and disorders of the French Bulldog population under primary veterinary care in the UK in 2013. Canine Genet. Epidemiol. 5, 3. O’Neill, D. G., Packer, R. M. A., Francis, P., Church, D. B., Brodbelt, D. C. and Pegram, C. 2021. French Bulldogs differ to other dogs in the UK in propensity for many common disorders: a VetCompass study. Canine Med. Genet. 8, 13. Rohrer Bley, C., Staudinger, C., Bley, T., Marconato, L., Sabattini, S. and Beckmann, K. 2022. Canine presumed glial brain tumours treated with radiotherapy: Is there an inferior outcome in tumours contacting the subventricular zone? Vet. Comp. Oncol. 20, 29-37. Rossmeisl, J. H., & Pancotto, T. E. 2020. Tumors of the Nervous System. In Withrow and MacEwen’s small animal clinical oncology, 6th ed. Ed., Vail, D.M., Thamm, D. H. and Liptak, J.: St.Louis, MO: Elsevier, pp: 657−674. Schwarz, P., Meier, V., Soukup, A., Drees, R., Besserer, J., Beckmann, K., Roos, M. and Rohrer Bley, C. 2018. Comparative evaluation of a novel, moderately hypofractionated radiation protocol in 56 dogs with symptomatic intracranial neoplasia. J. Vet. Intern. Med. 32, 2013-2020. Snyder, J. M., Shofer, F. S., Van Winkle, T. J. and Massicotte, C. 2006. Canine intracranial primary neoplasia: 173 cases (1986-2003). J. Vet. Intern. Med. 203, 669-675. Song, R. B., Vite, C. H., Bradley, C. W. and Cross, J. R. 2013. Postmortem evaluation of 435 cases of intracranial neoplasia in dogs and relationship of neoplasm with breed, age, and body weight. J. Vet. Intern. Med. 27, 1143-1152. Tonogai, E. J., Huang, S., Botham, R. C., Berry, M. R., Joslyn, S. K., Daniel, G. B., Chen, Z., Rao, J., Zhang, X., Basuli, F., Rossmeisl, J.H., Riggins, G.J., LeBlanc, A.K., Fan, T.M. and Hergenrother, P. J. 2021. Evaluation of a procaspase-3 activator with hydroxyurea or temozolomide against high-grade meningioma in cell culture and canine cancer patients. Neuro. Oncol. 23, 1723-1735. Treggiari, E., Maddox, T. W., Gonçalves, R., Benoit, J., Buchholz, J. and Blackwood, L. 2017. Retrospective comparison of three-dimensional conformal radiation therapy vs. predonisolone alone in 30 cases of canine intracranial brain tumors. Vet. Radiol. Ultrasound 58, 106-116. Van Asselt, N., Christensen, N., Meier, V., Rohrer Bley, C., Laliberte, S., Poirier, V. J., Desai, N., Chen, Y. and Turek, M. 2020. Definitive-intent intensity-modulated radiation therapy provides similar outcomes to those previously published for definitive-intent three-dimensional conformal radiation therapy in dogs with primary brain tumors: A multi-institutional retrospective study. Vet. Radiol. Ultrasound, 61, 481-489. Vigeral, M., Bentley, R. T., Rancilio, N. J., Miller, M. A. and Heng, H. G. (2018). Antemortem detection of oligodendroglioma “cerebrospinal fluid drop metastases” in a dog by serial magnetic resonance imaging. Vet. Radiol. Ultrasound 59, E32-E37. | ||
| How to Cite this Article |
| Pubmed Style Nakaichi M, Nemoto Y, Iseri T, Itoh H, Sunahara H, Itamoto T, Itamoto K, Tani K. Possible involvement of cerebrospinal fluid drop metastasis in the survival of French bulldogs after radiotherapy for presumed glial brain tumors. Open Vet. J.. 2025; 15(9): 4592-4600. doi:10.5455/OVJ.2025.v15.i9.65 Web Style Nakaichi M, Nemoto Y, Iseri T, Itoh H, Sunahara H, Itamoto T, Itamoto K, Tani K. Possible involvement of cerebrospinal fluid drop metastasis in the survival of French bulldogs after radiotherapy for presumed glial brain tumors. https://www.openveterinaryjournal.com/?mno=252563 [Access: January 25, 2026]. doi:10.5455/OVJ.2025.v15.i9.65 AMA (American Medical Association) Style Nakaichi M, Nemoto Y, Iseri T, Itoh H, Sunahara H, Itamoto T, Itamoto K, Tani K. Possible involvement of cerebrospinal fluid drop metastasis in the survival of French bulldogs after radiotherapy for presumed glial brain tumors. Open Vet. J.. 2025; 15(9): 4592-4600. doi:10.5455/OVJ.2025.v15.i9.65 Vancouver/ICMJE Style Nakaichi M, Nemoto Y, Iseri T, Itoh H, Sunahara H, Itamoto T, Itamoto K, Tani K. Possible involvement of cerebrospinal fluid drop metastasis in the survival of French bulldogs after radiotherapy for presumed glial brain tumors. Open Vet. J.. (2025), [cited January 25, 2026]; 15(9): 4592-4600. doi:10.5455/OVJ.2025.v15.i9.65 Harvard Style Nakaichi, M., Nemoto, . Y., Iseri, . T., Itoh, . H., Sunahara, . H., Itamoto, . T., Itamoto, . K. & Tani, . K. (2025) Possible involvement of cerebrospinal fluid drop metastasis in the survival of French bulldogs after radiotherapy for presumed glial brain tumors. Open Vet. J., 15 (9), 4592-4600. doi:10.5455/OVJ.2025.v15.i9.65 Turabian Style Nakaichi, Munekazu, Yuki Nemoto, Toshie Iseri, Harumichi Itoh, Hiroshi Sunahara, Takuya Itamoto, Kazuhito Itamoto, and Kenji Tani. 2025. Possible involvement of cerebrospinal fluid drop metastasis in the survival of French bulldogs after radiotherapy for presumed glial brain tumors. Open Veterinary Journal, 15 (9), 4592-4600. doi:10.5455/OVJ.2025.v15.i9.65 Chicago Style Nakaichi, Munekazu, Yuki Nemoto, Toshie Iseri, Harumichi Itoh, Hiroshi Sunahara, Takuya Itamoto, Kazuhito Itamoto, and Kenji Tani. "Possible involvement of cerebrospinal fluid drop metastasis in the survival of French bulldogs after radiotherapy for presumed glial brain tumors." Open Veterinary Journal 15 (2025), 4592-4600. doi:10.5455/OVJ.2025.v15.i9.65 MLA (The Modern Language Association) Style Nakaichi, Munekazu, Yuki Nemoto, Toshie Iseri, Harumichi Itoh, Hiroshi Sunahara, Takuya Itamoto, Kazuhito Itamoto, and Kenji Tani. "Possible involvement of cerebrospinal fluid drop metastasis in the survival of French bulldogs after radiotherapy for presumed glial brain tumors." Open Veterinary Journal 15.9 (2025), 4592-4600. Print. doi:10.5455/OVJ.2025.v15.i9.65 APA (American Psychological Association) Style Nakaichi, M., Nemoto, . Y., Iseri, . T., Itoh, . H., Sunahara, . H., Itamoto, . T., Itamoto, . K. & Tani, . K. (2025) Possible involvement of cerebrospinal fluid drop metastasis in the survival of French bulldogs after radiotherapy for presumed glial brain tumors. Open Veterinary Journal, 15 (9), 4592-4600. doi:10.5455/OVJ.2025.v15.i9.65 |