| Case Report | ||
Open Vet. J.. 2025; 15(5): 2277-2282 Open Veterinary Journal, (2025), Vol. 15(5): 2277-2282 Case Report Vitamin K deficiency as a cause of oral bleeding in a dog with intestinal malabsorption due to lymphocytic-plasmacytic enteritisGiulia Marceglia* and Matteo PetiniSan Marco Veterinary Clinic, Padova, Italy *Corresponding Author: Giulia Marceglia. San Marco Veterinary Clinic, Padova, Italy. Email: giuliamarceglia04 [at] gmail.com Submitted: 18/03/2025 Revised: 14/04/2025 Accepted: 18/04/2025 Published: 31/05/2025 © 2025 Open Veterinary Journal
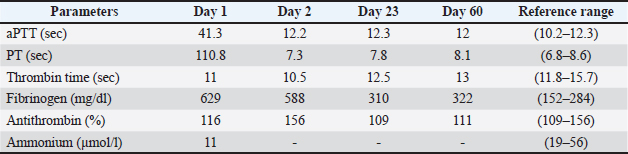
ABSTRACTBackground: Vitamin K, a member of the fat-soluble vitamin group, plays a key role in hemostasis by facilitating the activation of vitamin K-dependent clotting factors and contributing to the synthesis of various coagulation proteins. Consequently, its antagonization or deficiency secondary to reduced production or malabsorption impairs coagulation, leading to an increased risk of bleeding. Case Description: A 4-year-old, intact female German Shepherd was referred for a year-long history of anorexia, intermittent vomiting, and chronic diarrhea. She developed oral bleeding over the past 2 days. Diagnostic investigations revealed markedly prolonged prothrombin time (PT) and activated partial thromboplastin times (aPTT) with normal plasma fibrinogen levels. These findings, in conjunction with the normalization of PT and aPTT following vitamin K1 administration and the exclusion of rodenticide or coumarin intoxication, suggested vitamin K deficiency secondary to intestinal malabsorption. Further investigation led to the diagnosis of severe lymphoplasmacytic enterocolitis. Conclusion: Vitamin K-responsive coagulopathy associated with malabsorption syndrome secondary to lymphocytic-plasmacytic enteritis was previously described in two cats, but this is the first report of its occurrence in a dog. Therefore, vitamin K supplementation should be considered in all animals with intestinal malabsorption. Keywords: Vitamin K, Coagulation, Lymphocytic-plasmacytic enteritis, Dog. IntroductionVitamins are a group of biochemically distinct families of organic compounds that are required in small amounts for metabolic processes (Chipponi et al., 1982). Vitamins can be divided into water-soluble and fat-soluble vitamins (Pazirandeh and Burns, 2017), and vitamin K is included in the latter group (Gallop et al., 1980). Specifically, Vitamin K consists of two main forms: phylloquinone (vitamin K1), which is predominantly found in plants, especially in green leafy vegetables, and menaquinone (vitamin K2), which is mainly produced by certain intestinal bacteria, although it is also present in small quantities in animal-derived foods (Matthaiou et al., 2023). A wide range of facultative or obligate anaerobic bacteria in the intestine, including Escherichia coli, Bacteroides fragilis, Eggerthella lenta, and Lactococcus lactis, are responsible for producing various menaquinone subtypes. For this reason, disruption of the intestinal microbiota, such as dysbiosis, can adversely affect the production of these compounds (Pazirandeh and Burns, 2017; Kemp et al., 2022). As lipid-soluble compounds, proper functioning of the hepatobiliary system, pancreas, and intestine is essential for the effective absorption of vitamin K (Matthaiou et al., 2023). When ingested, vitamin K1 binds to proteins that are broken down by pancreatic enzymes in the small intestine. Both free vitamin K1 from food and vitamin K2 produced by gut bacteria are solubilized into micelles with the help of bile salts. These micelles are then absorbed by enterocytes, incorporated into chylomicrons, and then transported through the lymphatic system to directly reach the liver (Pazirandeh and Burns, 2017). Vitamin K plays a crucial role in maintaining coagulation balance. The hydroquinone form of vitamin K serves as a cofactor for the enzyme gamma-glutamyl carboxylase, which catalyzes the γ-carboxylation of glutamic acid residues on various proteins involved in the coagulation process. These proteins include factors II, VII, IX, and X, as well as proteins C, S, and Z, which are converted into their active forms. This reaction also requires molecular oxygen and carbon dioxide, with one molecule of vitamin K epoxide being produced for each glutamic acid residue that undergoes carboxylation. As a result, vitamin K deficiency is primarily linked to impaired coagulation and an increased tendency to bleed (Furie et al.,1999; Berkner, 2005). The purpose of this report was to describe the clinical history, laboratory data, and pathologic features of a dog with chronic lymphocytic-plasmacytic enteritis and suspected vitamin K-deficient hemorrhagic diathesis. Case DetailsA 4-year-old intact female German Shepherd was referred to the San Marco Veterinary clinic with a 1-year history of reduced appetite, intermittent vomiting, and chronic diarrhea. In the past 2 days, she also developed oral bleeding. The dog was fully vaccinated and treated for ecto- and endoparasites. There was no known access to toxins. She was on a hyperdigestive commercial diet. Upon presentation, the patient was mentally dull, she had severe diffuse muscle wast, and a body condition score of 1 out of 9. The patient had pale mucous membranes with prolonged capillary refill time and bleeding gums. The heart rate was normal (144 beats/min) with palpable femoral pulses. The systolic blood pressure measured by the oscillometric method was 133 mmHg. Her body temperature was 37.2°C. The abdomen was uncomfortable during palpation. The rest of the physical examination was unremarkable. The main findings from the complete blood count (CBC) were moderate regenerative anemia and slight thrombocytopenia (Table 1, day 1). Serum biochemistry revealed a slight elevation of alanine aminotransferase, mild panhypoprotidemia, moderate hypocholesterolemia, and a slight increase in serum lactate (Table 2, day 1). Considering that the degree of thrombocytopenia did not explain the oral bleeding, a coagulation panel was performed. The results showed severe prolongation of both prothrombin time (PT) and activated partial thromboplastin time (aPTT) (Table 3, day 1). The dog was hospitalized; the initial stabilization included the administration of vitamin K1 (Vitamina K1, Laboratoire TVM 50 mg) (5 mg/kg intravenously once, then 2.5 mg/kg PO q 12 hours), along with a whole blood transfusion (15 ml/kg) due to the combination of early signs of shock and coagulopathy. A toxicology screening for anticoagulant rodenticides and coumarins by liquid chromatography with tandem mass spectrometry (Bertolini et al., 2024) was requested. The result was a negative ruling out acquired coagulopathy caused by vitamin K1 antagonist ingestion. Repeated PT and aPTT testing 24 hours after vitamin K1 showed a complete normalization of both coagulation times, and no further oral bleeding was observed. At this point, the conditions leading to vitamin K1 deficiency were considered. Based on a history of chronic gastrointestinal signs, weight loss, and the combination of hypocholesterolemia and panhypoprotidemia, intestinal malabsorption was the most likely cause of vitamin K1 deficiency. Pancreatic insufficiency was excluded based on normal canine trypsin-like immunoreactivity (24; reference 5.2–35 µg/l). Hypocobalaminemia (100 ng/l; reference 290–611 ng/l) further supported the diagnosis of intestinal malabsorption despite normal serum folate levels (5.6 µg/l; reference 3.0–15 µg/l). The fecal sample was negative for parasitic diseases and Giardia spp. Abdominal ultrasound showed mild and nonspecific signs of enteropathy (Fig. 1). No other abnormalities were detected. Supplementation with cyanocobalamin (Dobetin B1, 10000, Ecuphar Italia) was started subcutaneously (1,500 mcg) with further administration at the same dosage once a week for 6 weeks. After 3 days of hospitalization, the patient was discharged with Vitamin K1 2.5 mg/kg PO twice daily, probiotics (Vivomixx 450 miliardi di batteri, Biosphaera Pharma S.r.l.) (1 sachet once daily), and a hydrolyzed commercial diet. Table 1. Total cells blood count of the patient at the time of presentation and on day 23.
Table 2. Biochemistry of the patient at the time of presentation and on day 23.
Table 3. Coagulative panel and blood ammonia of the patient at the time of presentation and on days 2, 23 and 60
Fig. 1. Abdominal ultrasound of the gastro-intestinal tract. The stomach is moderately distended by gas. The gastric wall appears altered due to the prominence of the submucosal layer (A). Multiple fluid-filled jejunal loops are observed; intestinal wall alterations include: slight thinning and hyperechogenicity of the mucosal layer (B). Twenty days after discharge, the patient returned for a recheck examination. The owners reported persistent diarrhea and weight loss. The CBC revealed resolution of anemia and moderate thrombocytosis (Table 1, days 23), while the biochemistry revealed persistent hypoalbuminemia and hypocholesterolemia (Table 2, days 23). The coagulation panel was normal (Table 3, days 23); thus, vitamin K1 supplementation was discontinued. The repeated abdominal ultrasound showed no significant changes compared with the previous examination. Considering the lack of improvement in the clinical condition, endoscopy of the upper and lower gastrointestinal tract with multiple biopsies sampling was recommended. The histopathological diagnosis was of a chronic lymphocytic-plasmacytic gastritis and chronic lymphocytic-plasmacytic enterocolitis; moderate dilation of the lymphatic vessels was also observed in the duodenal biopsies (Fig. 2). At this point, immunosuppressive therapy with prednisolone (Prednicortone 20 mg, Dechra Veterinary Products S.r.l.) was started at a dose of 2 mg/kg once daily. Over the next 4 weeks, the owner noticed no further gastrointestinal or bleeding signs, and an increase in body weight was also observed. Prednisolone tapering was initiated 8 weeks after the start of treatment, with the dosage reduced from 2 mg/kg PO every 24 hours to 1.5 mg/kg PO every 24 hours. However, the dog experienced a recurrence of diarrhea and weight loss, prompting the initiation of a second immunosuppressive therapy with cyclosporine (Cyclavance 100 mg/ml, Virbac) (5 mg/kg q12h). Despite the uncontrolled gastrointestinal signs, the dog did not experience any recurrence of the clinical bleeding or prolongation of clotting times (Table 3, day 60).
Fig. 2. Hematoxylin and eosin-stained biopsy specimen of the duodenum. Multifocal fusion of the villous tips, some of which have a blunted profile and are slightly to moderately shortened. The lymphatic vessels are characterized by dilatation of varying degrees, from mild/moderate to occasionally severe. The lamina propria is characterized by a moderate increase in the number of small mature lymphocytes and plasma cells, as well as a mild increase in the number of infiltrating eosinophils. It is associated with moderate and multifocal-coalescing interstitial edema (A). Hematoxylin and eosin-stained biopsy specimen of colon. The lamina propria is characterized by mild-to-moderate increases in lymphocytes, plasma cells, and multifocally infiltrating neutrophilic granulocytes. Rarely do the crypts present with a dilated lumen containing desquamated cells, weakly eosinophilic material, and few neutrophilic granulocytes. Multifocal interstitial edema is associated. Finally, multifocal erosion of the superficial epithelium are observed (B). Over the following 6 months, the dog failed to improve despite multiple dietary interventions, immunosuppressive therapy modulation, and fecal transplant. The dog was ultimately euthanized. DiscussionThe present study describes a dog with a bleeding tendency and a history of chronic gastro-intestinal signs. In this case, the combination of prolonged PT and aPTT with normal fibrinogen concentrations raised suspicion of vitamin K antagonist ingestion or vitamin K deficiency. The dog had no history of exposure to toxins or anticoagulant medications; furthermore, the liquid chromatography-mass spectrometry analysis performed on the blood did not detect any trace of these compounds in the patient. Because this test is the most reliable method for confirming exposure to rodenticides (Hunter et al., 1988; Bertolini et al., 2024), the likelihood of a false negative result was negligible. Consequently, rodenticide intoxication was reasonably ruled out as a possible cause of bleeding in this dog. The initial elevation in aminotransferase levels in this case could have suggested liver disease as a cause of vitamin K deficiency. However, the absence of laboratory findings indicating liver dysfunction (e.g., hyperbilirubinemia and hyperammonemia) and a normal fibrinogen serum level weakened this hypothesis. Certainly, performing a serum bile acid stimulation test could have helped more confidently to exclude liver insufficiency, but this test was not performed. Cholestatic disease due to extrahepatic biliary tract obstruction is another mechanism of vitamin K deficiency due to malabsorption (Blois, 2024). However, based on the clinical presentation, as well as the laboratory (e.g., normal serum bilirubin) and imaging findings, this association was deemed improbable in our patient. In addition, in a previous study, no dogs with partial or complete extrahepatic biliary obstruction exhibited prolonged PT or aPTT, suggesting adequate vitamin K absorption (Mayhew et al., 2013). In this case, vitamin deficiency, causing oral bleeding, was attributed to intestinal malabsorption due to enterocolitis. In addition, the state of deficiency in the patient could have been complicated by several conditions related to intestinal microbioma disruption, such as a decreased number of menaquinone-producing bacteria and an overgrowth of vitamin K-consuming microorganisms. The normal trypsin-like immunoreactivity allows to consider a primary intestinal disease as the cause of this condition. Spontaneous bleeding secondary to vitamin K, though rare, is a well-documented complication of intestinal malabsorption in humans and especially in infants (Kark et al., 1940; Moore et al., 1956; Schoon et al., 2001; Araki and Shirahata, 2020; Kocic et al., 2023). Human studies have shown that conditions affecting the absorption of dietary fats, such as intestinal lymphangiectasia and chronic inflammatory bowel disease, may lead to deficiencies in fat-soluble vitamins (Farraye et al., 2011; Fabisiak et al., 2017; Ghishan and Kiela, 2017). Similar findings have been recently reported in dogs with chronic enteropathy, although not specifically for vitamin K (Serafini et al., 2024). Because vitamin K is a fat-soluble vitamin, its deficiency could be expected in these cases. However, to the best of our knowledge, this has not been specifically investigated. Nevertheless, hypocoagulability in dogs with protein-losing enteropathy might be linked to vitamin K deficiency due to intestinal malabsorption (Blois, 2024). Again, the authors found no studies reporting the frequencies of bleeding events in dogs with intestinal malabsorption, and in the available veterinary literature, this complication has been reported in two cats with malabsorption syndrome secondary to lymphocytic plasmocytic enteritis (Edwards and Russell, 1987). Although prolonged PT and aPTT with normal fibrinogen concentrations may suggest vitamin K deficiency, they are not reliable biomarkers for diagnosing vitamin K deficiency precisely. This is because these clotting times only measure the vitamin K used by the liver for the synthesis of coagulation factors. The remaining vitamin K is used for bone metabolism (Kuwabara et al., 2009). In humans, it is well known that vitamin K deficiency affects bone metabolism first before causing any blood clotting problems. For this reason, a significant deficiency of vitamin K must occur for PT to increase and lead to bleeding events (Vernia et al., 2023). This could explain why bleeding events are rarely reported in humans or even unnoticed in small animals. In the present case, after supplementation with vitamin K1 no more bleeding events were noticed by the patient, nor were they detected during the patient’s reevaluation. Additionally, abnormal clotting times were not observed in the subsequent coagulation test, despite the interruption of vitamin K1 supplementation and persistence of gastrointestinal signs. It is possible that the administration of oral vitamin K1 might have increased the body’s stores for an extended period before clotting factors became deficient again. This case suggests that vitamin K treatment should be considered in all animals with intestinal malabsorption, particularly when abnormal clotting is detected or before procedures associated with bleeding risk. AcknowledgmentsNone. Conflict of interestThe authors declare that they have no conflicts of interest. FundingThis study was not supported by any sponsor or funder. Authors’ contributionsGiulia Marceglia wrote the manuscript with the contribution of Matteo Petini. Both authors have contributed to the revision and the writing of the article, and approved the final version. Data availabilityThe data supporting the findings of this case report are available upon reasonable request from the corresponding author. ReferencesAraki, S. and Shirahata, A. 2020. Vitamin k deficiency bleeding in infancy. Nutrients 12(3), 78. Berkner, K.L. 2005. The vitamin K-dependent carboxylase. Annu. Rev. Nutr. 25, 127–149. Bertolini, F.M., Barolo, E., Masti, R., De Arcangeli, S., Furlanello, T., Ongaro, V., Meneghini, C. and Sanchez del Pulgar, J. 2024. Fast and sensitive method for the diagnosis and follow-up of anticoagulant rodenticides poisoning in animal whole blood. J. Chromatogr. B. Analyt Technol. Biomed. Life Sci. 1, 1232,1–8. Blois, S.L. 2024. Hyper- and hypocoagulable states. In Ettinger’ s textbook of veterinary internal medicine. Eds., Cote, E., Ettinger, S.J. and Feldman, E.C. Philadelphia, PA: Elsevier Science Health Science, pp: 863–869. Chipponi, J.X., Bleier, J.C., Santi, M.T. and Rudman, D. 1982. Deficiencies of essential and conditionally essential nutrients. Am. J. Clin. Nutr. 35(5), 1112–1116. Edwards, D.F. and Russell, R.G. 1987. Probable vitamin K-deficient bleeding in two cats with malabsorption syndrome secondary to lymphocytic plasmacytic enteritis. J. Vet. Intern. Med. 1(3), 97–101. Fabisiak, N., Fabisiak, A., Watala, C. and Fichna, J. 2017. Fat-soluble vitamin deficiencies and inflammatory bowel disease: systematic review and meta-analysis. J. Clin. Gastroenterol. 51(10), 878–889. Farraye, F.A., Nimitphong, H., Stucchi, A., Dendrinos, K., Boulanger, A.B., Vijjeswarapu, A., Tanennbaum, A., Biancuzzo, R., Chen, T.C. and Holick, M.F. 2011. Use of a novel vitamin D bioavailability test demonstrates that vitamin D absorption is decreased in patients with quiescent crohn’s disease. Inflamm. Bowel Dis. 17, 2116–2121. Furie, B., Bouchard, B.A. and Furie, B.C. 1999. Vitamin K-dependent biosynthesis of-carboxyglutamic acid. Blood 93(6), 1798–1808. Gallop, P.M., William, J.B. and Haushka, P.V. 1980. Carboxylated calcium-binding proteins and vitamin K. N. Eng. J. Med. 302(26), 1460–1466. Ghishan, F.K. and Kiela, P.R. 2017. Vitamins and minerals in inflammatory bowel disease. Gastroenterol. Clin. North Am. 46(4), 797–808. Hunter, K., Sharp, E.A. and Newton, A. 1988. Determination of diastereoisomers of bromadiolone, an anticoagulant rodenticide, in animal tissue by high-performance liquid chromatography. J. Chromatography. 435(1), 83–95. Kark, R.M., Souter, A. and Hayward, J.C. 1940. A haemorrhagic diathesis in idiopathic steatorrhea: observations on its association with vitamin K deficiency. Q. J. Med. 9, 247–261. Kemp, J.A., Alvarenga, L., Cardozo, L.F.M.F., Dai, L., Stenvinkel, P., Shiels, P.G., Hackeng, T.M., Schurgers, L.J. and Mafra, D. 2022. Dysbiosis in patients with chronic kidney disease: let us talk about vitamin K. Curr. Nutr. Rep. 11(4), 765–779. Kocic, M., Prokic, D., Kitic, I., Rasic, P., Savic, D., Milickovic, M., Mijovic, T., Marusic, V. and Sarajlija, A. 2023. Age-specific causes of upper gastrointestinal bleeding in children. World J. Gastroenterol. 29(47), 6095–6110. Kuwabara, A., Tanaka, K., Tsugawa, N., Nakase, H., Tsuji, H., Shide, K., Kamao, M., Chiba, T., Inagaki, N., Okano, T. and Kido, S. 2009. High prevalence of vitamin K and D deficiency and decreased BMD in inflammatory bowel disease. Osteoporos. Int. 20, 935–942. Matthaiou, A.M., Tomos, I., Chaniotaki, S., Liakopoulos, D., Sakellaropoulou, K., Koukidou, S., Gheorghe, L.M., Eskioglou, S., Paspalli, A., Hillas, G. and Dimakou, K. 2023. Association of broad-spectrum antibiotic therapy and vitamin E supplementation with vitamin K deficiency-induced coagulopathy: a case report and narrative review of the literature. J. Pers. Med. 13(9), 1349–1360. Mayhew, P.D., Savigny, M.R., Otto, M.C., Brown, D.C., Brooks, M.B., Bentley, A.M., Runge, J.J. and Callan, M.B. 2013. Evaluation of coagulation in dogs with partial or complete extrahepatic biliary tract obstruction by means of thromboelastography. J. Am. Vet. Med. Assoc. 242(6), 778–785. Moore, M.J., Strickland, W.H. and Prichard, R.W. 1956. Sprue with bleeding from hypoprothrombinemia. Arch. Intern. Med. 97(6), 814–816. Pazirandeh, S. and Burns, D.L. 2017. Overview of vitamin-K. UptoDate 1–17. Schoon, E.J., Müller, C.A., Vermeer, C., Schurgers, L.J., Brummer, R.J. and Stockbrügger, R.W. 2001. Low serum and bone vitamin K status in patients with longstanding Crohn’s disease: another pathogenetic factor of osteoporosis in Crohn’s disease? Gut 48(4), 473–477. Serafini, F., Maxwell, K.M., Zhu, X. and Lennon, E.M. 2024. Dysregulated serum concentrations of fat-soluble vitamins in dogs with chronic enteropathy. J. Vet. Intern. Med. 38(5), 2612–2619. Vernia, F., Burrelli Scotti, G., Bertetti, N.S., Donato, G., Necozione, S., Vernia, P. and Pallotta, N. 2023. Low vitamin K and vitamin D dietary intake in patients with inflammatory bowel diseases. Nutrients 15(7), 1678–1690. | ||
| How to Cite this Article |
| Pubmed Style Marceglia G, Petini M. Vitamin K deficiency as a cause of oral bleeding in a dog with intestinal malabsorption due to lymphocytic-plasmacytic enteritis. Open Vet. J.. 2025; 15(5): 2277-2282. doi:10.5455/OVJ.2025.v15.i5.46 Web Style Marceglia G, Petini M. Vitamin K deficiency as a cause of oral bleeding in a dog with intestinal malabsorption due to lymphocytic-plasmacytic enteritis. https://www.openveterinaryjournal.com/?mno=248096 [Access: January 25, 2026]. doi:10.5455/OVJ.2025.v15.i5.46 AMA (American Medical Association) Style Marceglia G, Petini M. Vitamin K deficiency as a cause of oral bleeding in a dog with intestinal malabsorption due to lymphocytic-plasmacytic enteritis. Open Vet. J.. 2025; 15(5): 2277-2282. doi:10.5455/OVJ.2025.v15.i5.46 Vancouver/ICMJE Style Marceglia G, Petini M. Vitamin K deficiency as a cause of oral bleeding in a dog with intestinal malabsorption due to lymphocytic-plasmacytic enteritis. Open Vet. J.. (2025), [cited January 25, 2026]; 15(5): 2277-2282. doi:10.5455/OVJ.2025.v15.i5.46 Harvard Style Marceglia, G. & Petini, . M. (2025) Vitamin K deficiency as a cause of oral bleeding in a dog with intestinal malabsorption due to lymphocytic-plasmacytic enteritis. Open Vet. J., 15 (5), 2277-2282. doi:10.5455/OVJ.2025.v15.i5.46 Turabian Style Marceglia, Giulia, and Matteo Petini. 2025. Vitamin K deficiency as a cause of oral bleeding in a dog with intestinal malabsorption due to lymphocytic-plasmacytic enteritis. Open Veterinary Journal, 15 (5), 2277-2282. doi:10.5455/OVJ.2025.v15.i5.46 Chicago Style Marceglia, Giulia, and Matteo Petini. "Vitamin K deficiency as a cause of oral bleeding in a dog with intestinal malabsorption due to lymphocytic-plasmacytic enteritis." Open Veterinary Journal 15 (2025), 2277-2282. doi:10.5455/OVJ.2025.v15.i5.46 MLA (The Modern Language Association) Style Marceglia, Giulia, and Matteo Petini. "Vitamin K deficiency as a cause of oral bleeding in a dog with intestinal malabsorption due to lymphocytic-plasmacytic enteritis." Open Veterinary Journal 15.5 (2025), 2277-2282. Print. doi:10.5455/OVJ.2025.v15.i5.46 APA (American Psychological Association) Style Marceglia, G. & Petini, . M. (2025) Vitamin K deficiency as a cause of oral bleeding in a dog with intestinal malabsorption due to lymphocytic-plasmacytic enteritis. Open Veterinary Journal, 15 (5), 2277-2282. doi:10.5455/OVJ.2025.v15.i5.46 |