| Case Report | ||
Open Vet J. 2023; 13(3): 382-387 Open Veterinary Journal, (2023), Vol. 13(3): 382–387 Case Report A rare case report of extensive mandibular osteoma corrected by unilateral mandibulectomy: Cytological, radiological, and pathological investigationAmirhossein Alizadeh Tabarestani1, Masoud Nemati-Nezhad2, Mohammad Amin Minaie3, Sonia Sahvieh4,5 and Reza Nikzad6,7*1Faculty of Radiology Department, Islamic Azad University of Babol, Babol, Iran 2Board-Certified in Veterinary Clinical Pathology, School of Veterinary Medicine, Shiraz University, Shiraz, Iran 3Small Animal Internal Medicine, Doctor Hasanzadeh Specialized Veterinary Hospital, Babolsar, Iran 4Department of Pathology, School of Veterinary Medicine, Shiraz University, Shiraz, Iran 5Faculty of Pathology Department, Islamic Azad University of Babol, Babol, Iran 6Postgraduate in Veterinary Surgery, Shahid Bahonar University of Kerman, Kerman, Iran 7Member of National Elite Foundation of Iran *Corresponding Author: Reza Nikzad. Postgraduate in Veterinary Surgery, Shahid Bahonar University of Kerman, Kerman, Iran Email: rezanikzad [at] hotmail.com. Submitted: 02/01/2023 Accepted: 16/02/2023 Published: 22/03/2023 © 2023 Open Veterinary Journal
AbstractBackground: Osteoma is a benign bone tumor that rarely affects animals. The most common bones involved with this tumor included the mandible, maxillofacial bones, and nasal sinuses. Definitive diagnosis is based on pathology findings which allow for differentiation with other bone lesions. Case Description: The patient, a 5-year-old intact male Mongrel dog presented with a huge mandibular mass that involved both the right and left mandible, and led to dental occlusion. The radiography was performed and depicted the intense mass with a well-demarcated edge, a short transitional zone between normal and abnormal bone, and a smooth rounded radiopaque appearance. The investigation according to the fine needle aspiration showed the presence of oval to spindle shape cells with poorly malignancy criteria, fatty cells, reactive osteoblasts, and osteoclasts based on a population of spindle-shaped cells, and low numbers of degenerated neutrophils, bacteria, and few macrophages. Then, the radiographic assessments and cytology findings demonstrated the osteoma and were referred for surgical intervention. A unilateral mandibulectomy was performed, and the lesion was sent to the histopathology laboratory. The histopathology evaluation showed osteocyte proliferation without malignancy features. The osteoblast cells also showed no atypical proliferation that endorses the osteoma tumor. Conclusion: Although mandibular and maxillofacial bone resection in small animals have different tolerations, this patient became a candidate for surgery for future better nutrition and prevention of facial deformity and dental malocclusion. Follow-up after osteoma is one of the most necessary post-operation treatments to check the regeneration of the mass. There are considerable data in this report that should regard this tumor as a possible differential diagnosis for mandibular tumors. Keywords: Osteoma, Mandibulectomy, Bone, Dog, Histopathology. IntroductionOral neoplasms are the fourth most common neoplasia in dogs and, approximately seven percent of all tumors in this animal (Priester and McKay, 1980; Hoyt, 1984). Many factors contribute to the diagnosis of the masses as sex, breed, location, growth pattern, bone involvement, vessel invasion, lymph node invasion, metastasis, and recurrence (Simons, 2015). Osteoma is a benign tumor of bone (trabecular or dense lamellar) tissue (Van Duijl et al., 2018). They do not invade the cortical surface or undergo neoplastic changes. In humans, osteoma is specified as central, peripheral, and extra-skeletal (Kye et al., 2012). Osteoma is reported in the non-osteoid organs such as the stomach (Woo et al., 2019), skin (osteoma cutis) (Fernandez et al., 2012), and tongue (lingual osteoma) (Goldschmidt and Thrall, 1985). The most significant region of the osteoma tumor is the maxillofacial bones, such as the mandible, maxillae, and nasal/frontal bone, and maxillofacial bones are more susceptible to osteoma formation (Ogbureke et al., 2007; Sadeghi et al., 2015; Khandelwal et al., 2016). The purpose of this study is to describe the mandibular osteoma in a 5-year-old dog undergoing a surgical procedure to remove this tumor by mandibulectomy. Also, this report explains the treatment modality for this patient against an associated mandibular osteoma bone tumor treatment. Case DetailsThe 5-year-old vaccinated male intact mongrel breed was referred to Hassanzadeh Specialized Pet-hospital with a huge mass on the mandibular bone. The owner declared the mass appeared over 5 months. The clinical presentation started with drooling, problems in chewing, opened mouth caused by mass distention, malocclusion in the right mandible, and face changes. The right mandibular canine and first premolar tooth were not observed, the second premolar tooth was dislocated and the maxillary canine on the same side was oriented rostrally. There were no signs of pain and the mass was firm and bony consistency. Also, there was a smaller mass on the right mandible with lower invasion and lack of changes in dental occlusion (Fig. 1). The differential diagnosis of the mentioned case predicts old malunion fractures, and bone tumors such as osteosarcoma, osteoma, osteoblastoma, ossifying fibroma, and osteomyelitis or exostoses. Other jaw soft tissue masses such as epulis, squamous cell carcinoma, and ameloblastoma have rejected the cause of the consistency and bone structure of the mass. Diagnostic imagingThe skull radiographs were performed in dorsoventral and lateral projection which showed the intense and well-demarcated edge with a short transitional zone between normal and abnormal bone. There was a smooth rounded radiopaque appearance rostral of bilateral mandibles. The right mass size measured 8 × 4 cm and prevent normal chewing. The left mass has no remarkable changes in radiology in comparison to the left mass. The periosteal reaction and invasion of the surrounding soft tissue were not seen. Thoracic radiographs did not indicate pulmonary metastasis (Fig. 2).
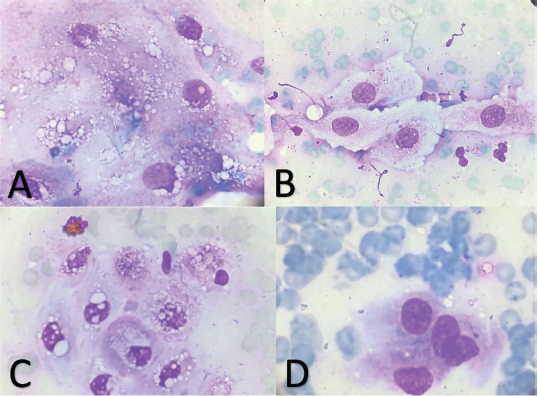
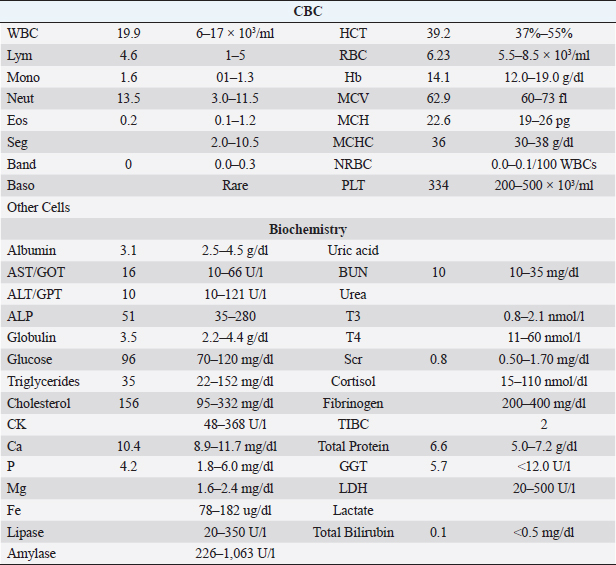
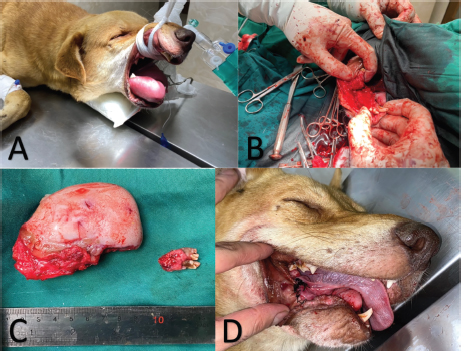
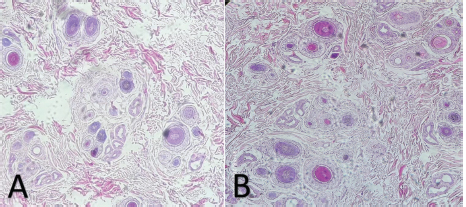
Fig. 1. (A–D) The huge mass on the mandibular bone was shown according to the clinical examination. Blood work and cytologyThe blood sample was collected and the leukogram showed mild neutrophilia and monocytosis which would be because of chronic inflammation. The biochemistry profile was normal and did not have a significant change (Table 1). Cytological assessment was performed by fine needle aspiration cytology from the core of the lesion. The microscopic evaluation showed oval to spindle shape cells with poorly malignancy criteria. A moderate number of fatty cells, degenerated neutrophils, bacteria, macrophages, osteoblasts, and osteoclasts. Septic inflammation was evident and suspected of mesenchymal tumor (Fig. 3). Surgical interventionDue to the chewing problem, mandibulectomy is considered the best treatment option for this patient. Therefore, the patient was sedated with Ketamine (5 mg/kg of body weight)-Diazepam (0.2 mg/kg of body weight), intravenously, and maintained by Isoflurane inhalation, respectively. It is positioned in the ventral recumbency and the mandibular mass is excised by unilateral mandibular ostectomy. The approach was according to the dissection of the Genioglossus, a superficial portion of the Masseter muscle, and the rostral portion of the Mylohyoideus muscle and Digastricus. Mandible was removed after the mandibular alveolar artery, vein, and inferior alveolar nerve ligation (Fig. 4). The antibiotic therapy (Cefazolin 25 mg/kg b.w., q8, 5 days and Clindamycin 11 mg/kg b.w. q24, 3 days) and analgesics (Morphine 0.2 mg/kg b.w.) were administrated. Pathologic descriptionThe mass was sent to the Histopathology Laboratory and the gross examination admitted a cream-tan tissue, measuring 10 × 5 cm2. The microscopic description revealed the admixture of mature lamellar and woven bone patterns, with Haversian-like canals. Cortical-type bone architecture is more frequent than trabecular bone architecture. Osteoblasts rimming bone are inconspicuous and small. Osteocytes in the matrix are small, not atypical, and randomly distributed. Intertrabecular marrow spaces are filled with moderately cellular and loose fibrous stroma. The final diagnosis was osteoma (Fig. 5).
Fig. 2. (A and C) Thoracic radiographs which are depicted there was no metastasis to the lungs. (B and D) The radiographs from the mandibular mass was performed.
Fig. 3. (A–D) The fine needle aspiration showed no cell abnormality. Table 1. Leukogram shows mild leukocytosis and monocytosis can be due to closed inflammation. CBT was normal.
Fig. 4. (A, B, and D) Tumor removal by surgery. (C) Gross morphology of mandibular mass. DiscussionOsteoma is an uncommon and rare benign primary bone neoplasm that often involved the maxillofacial, mandibles, and nasal sinuses. Due to the majority of bone tumors in animals being malignant (Quigley and Leedale, 1983), it is significant to diagnose the type of this tumor. Osteoma is a slow-growing lesion and is mostly diagnosed by the incident (Van Duijl et al., 2018). Mandibles are the most common location for this tumor (Larrea-Oyarbide et al., 2008). One of the common sites of osteoma formation is orbital osteoma, and in a study, orbital osteoma occurred in a 6-year-old male dog and was treated by surgical resection and medical therapy that include neomycin-polymyxinB-dexamethasone ophthalmic drops three times daily for 7 days with oral carprofen (2.2 mg/kg b.w.) four times daily during 7 days (Grozdanic et al., 2013). In the other study, frontal and parietal bone osteoma was resected surgically to reduce ophthalmic progressive complications and survived a lifetime of about 2 years without recurrence (Selmic et al., 2019). There are some approaches to the diagnosis of osteoma that included imaging methods (e.g., Computed tomography, Magnetic resonance imaging, or Scintigraphy), primary cytology, histopathology, and immunohistochemistry. If the patient is considered for surgical intervention, post-surgical pain management and nutrition manners in huge lesions are significant for patients candidates for mandibulectomy. The comprehension of this bone lesion etiology needs more studies based on many factors such as breed susceptibility, sex, age, and history of trauma (Dittmer and Pemberton, 2021). Further investigations are a necessity to elucidate the presumptive pathophysiological reasons for mandibular osteoma. Although, the mandibulectomy surgical procedure appears invasive approach for osteoma treatment, according to a study systemic non-steroidal anti-inflammatory drugs (NSAIDs) could regress the mass size and basic treatment, (Grozdanic et al., 2013) in this case, the cause of anorexia, is the refusal to eat due to inability to take food, and the preference of the patient’s client, mandibulectomy chosen as the treatment protocol. In fact, the authors also believe that other managements such as medical therapy, high-frequency ultrasound, and laser ablation could be a better option but many factors impress the judgment of future therapy such as patient’s status facilities availability, and owner expectations. In addition, the mandibulectomy complications should notice to enhance the quality of life after this surgical procedure.
Fig. 5. (A and B) Microscopic evaluation of the mandibular mass which is diagnosed as osteoma. ConclusionMandibular osteoma is a benign tumor in animals and the differential diagnosis should be considered between this tumor and the other mandibular masses including neoplastic or non-neoplastic lesions in dogs. In this study, we diagnosed this bone lesion as an osteoma according to the clinical examination, radiological assessment, clinical pathology, and histopathology findings and we performed the surgical procedure for curing this patient. However, this lesion was completely removed by mandibulectomy, and the contralateral mass was managed by NSAID medications, but the description of this case will be useful for veterinarians to designate this tumor as one of the differential diagnoses for the mandibular lesions. Conflict of interestThe authors declare that they have no competing interests. All data relevant to the study are included in the article. The authors have no conflict with data availability. FundingThere was no specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors. No funding was used in this study. ReferencesDittmer, K.E. and Pemberton, S. 2021. A holistic approach to bone tumors in dogs and cats: Radiographic and histologic correlation. Vet. Pathol. 58(5), 841–857. Fernandez, M., Grau-Roma, L., Roura, X. and Majó, N. 2012. Lingual osteoma in a dog. J. Small Anim. Pract. 53(8), 480–482. Hoyt, R.H. 1984. Oral malignancy in the dog. J. Am. Anim. Hosp. Assoc. 20, 83–91. Goldschmidt, M.H. and Thrall, D.E. 1985. Benign bone tumors in the dog. In Textbook of small animal orthopaedics. Eds., Newton C.D. and Nunamaker D.M. Philadelphia, PA: JB Lippincott Co, pp: 899–907. Grozdanic, S., Riedesel, E.A. and Ackermann, M.R. 2013. Successful medical treatment of an orbital osteoma in a dog: medical treatment of an orbital osteoma. Vet. Ophthalmol. 16(2), 135–139. Khandelwal, P., Dhupar, V. and Akkara, F. 2016. Unusually large peripheral osteoma of the mandible - A rare case report. J. Clin. Diagn. Res. 10(11), ZD11–ZD12. Kye, E.Y., Park, J.S., Ku, S.K., Yun, S.H., Oh, T.H., Lee, K.W., Kwon, Y.S. and Jang, K.H. 2012. Gastric osteoma in a dog. Pak. Vet. J. 32(1), 141–143. Larrea-Oyarbide, N., Valmaseda-Castellón, E., Berini-Aytés, L. and Gay-Escoda, C. 2008. Osteomas of the craniofacial region. Review of 106 cases: craniofacial osteomas. J. Oral Pathol. Med. 37(1), 38–42. Ogbureke, K.U.E., Nashed, M.N. and Ayoub, A.F. 2007. Huge peripheral osteoma of the mandible: a case report and review of the literature. Pathol. Res. Pract. 203(3), 185–188. Priester, W.A. and McKay, F.W. 1980. The occurrence of tumors in domestic animals. Natl. Cancer Inst. Monogr. 54, 1–210. Quigley, P.J. and Leedale, A.H. 1983. Tumors involving bone in the domestic cat: a review of fifty-eight cases. Vet. Pathol. 20(6), 670–686. Sadeghi, H.M., Shamloo, N., Taghavi, N., Safi, Y., Aghdashi, F. and Ismaeilnejad, M. 2015. Giant osteoma of mandible causing dyspnea: a rare case presentation and review of the literature. J. Maxillofac. Oral Surg. 14(3), 836–840. Selmic, L.E., Cray, M.T., Good, J.G., Hummel, D.W. and Joslyn, S. 2019. Modified lateral orbitotomy with combined partial zygomatic arch and vertical ramus ostectomies for excision of a frontal and parietal bone osteoma in a dog. Vet. Surg. 48(2), 257–262. Simons, K.W.J. 2015. Oral tumours in dogs: a retrospective study of 110 cases (2002-2014) (Utrecht Univ. (Master’s thesis). Van Duijl, J., Winer, J.N., De Rooster, H. and Arzi, B. 2018. Peripheral osteoma of the mandible in a cat. Vlaams Diergeneeskd Tijdschr. 87(2), 93–98. Woo, S.H., Go, D.M., Lee, S.H., Han, S.S. and Kim, D.Y. 2019. Primary osteoma cutis in the interscapular region of a dog. J. Comp. Pathol. 166, 1–4. | ||
| How to Cite this Article |
| Pubmed Style Tabarestani AA, Nejad MN, Minaie MA, Sahvieh S, Nikzad R. A rare case report of extensive mandibular osteoma corrected by unilateral mandibulectomy: Cytological, radiological, and pathological investigation. Open Vet J. 2023; 13(3): 382-387. doi:10.5455/OVJ.2023.v13.i3.16 Web Style Tabarestani AA, Nejad MN, Minaie MA, Sahvieh S, Nikzad R. A rare case report of extensive mandibular osteoma corrected by unilateral mandibulectomy: Cytological, radiological, and pathological investigation. https://www.openveterinaryjournal.com/?mno=93881 [Access: July 05, 2025]. doi:10.5455/OVJ.2023.v13.i3.16 AMA (American Medical Association) Style Tabarestani AA, Nejad MN, Minaie MA, Sahvieh S, Nikzad R. A rare case report of extensive mandibular osteoma corrected by unilateral mandibulectomy: Cytological, radiological, and pathological investigation. Open Vet J. 2023; 13(3): 382-387. doi:10.5455/OVJ.2023.v13.i3.16 Vancouver/ICMJE Style Tabarestani AA, Nejad MN, Minaie MA, Sahvieh S, Nikzad R. A rare case report of extensive mandibular osteoma corrected by unilateral mandibulectomy: Cytological, radiological, and pathological investigation. Open Vet J. (2023), [cited July 05, 2025]; 13(3): 382-387. doi:10.5455/OVJ.2023.v13.i3.16 Harvard Style Tabarestani, A. A., Nejad, . M. N., Minaie, . M. A., Sahvieh, . S. & Nikzad, . R. (2023) A rare case report of extensive mandibular osteoma corrected by unilateral mandibulectomy: Cytological, radiological, and pathological investigation. Open Vet J, 13 (3), 382-387. doi:10.5455/OVJ.2023.v13.i3.16 Turabian Style Tabarestani, Amirhossein Alizadeh, Masoud Nemati Nejad, Mohammad Amin Minaie, Sonia Sahvieh, and Reza Nikzad. 2023. A rare case report of extensive mandibular osteoma corrected by unilateral mandibulectomy: Cytological, radiological, and pathological investigation. Open Veterinary Journal, 13 (3), 382-387. doi:10.5455/OVJ.2023.v13.i3.16 Chicago Style Tabarestani, Amirhossein Alizadeh, Masoud Nemati Nejad, Mohammad Amin Minaie, Sonia Sahvieh, and Reza Nikzad. "A rare case report of extensive mandibular osteoma corrected by unilateral mandibulectomy: Cytological, radiological, and pathological investigation." Open Veterinary Journal 13 (2023), 382-387. doi:10.5455/OVJ.2023.v13.i3.16 MLA (The Modern Language Association) Style Tabarestani, Amirhossein Alizadeh, Masoud Nemati Nejad, Mohammad Amin Minaie, Sonia Sahvieh, and Reza Nikzad. "A rare case report of extensive mandibular osteoma corrected by unilateral mandibulectomy: Cytological, radiological, and pathological investigation." Open Veterinary Journal 13.3 (2023), 382-387. Print. doi:10.5455/OVJ.2023.v13.i3.16 APA (American Psychological Association) Style Tabarestani, A. A., Nejad, . M. N., Minaie, . M. A., Sahvieh, . S. & Nikzad, . R. (2023) A rare case report of extensive mandibular osteoma corrected by unilateral mandibulectomy: Cytological, radiological, and pathological investigation. Open Veterinary Journal, 13 (3), 382-387. doi:10.5455/OVJ.2023.v13.i3.16 |