| Case Report | ||
Open Vet J. 2022; 12(6): 864-867 Open Veterinary Journal, (2022), Vol. 12(6): 864–867 Case Report Urinary liver-type fatty acid-binding protein in two dogs with acquired Fanconi syndrome: A case reportSatoshi Takashima1, Tomomi Nasu1, Keiichi Ohata2,3, Tsuyoshi Oikawa2, Takeshi Sugaya3, Yui Kobatake1, Sanae Shibata1 and Naohito Nishii1*1Joint Department of Veterinary Medicine, Faculty of Applied Biological Sciences, Gifu University, Gifu, Japan 2CMIC Holdings Co., Ltd., Tokyo, Japan 3Division of Nephrology and Hypertension, Department of Internal Medicine, St. Marianna University School of Medicine, Kanagawa, Japan Submitted: 14/07/2022 Accepted: 20/10/2022 Published: 18/11/2022 *Corresponding Author: Naohito Nishii. Joint Department of Veterinary Medicine, Faculty of Applied Biological Sciences, Gifu University, Gifu, Japan. Email: nishii [at] gifu-u.ac.jp © 2022 Open Veterinary Journal
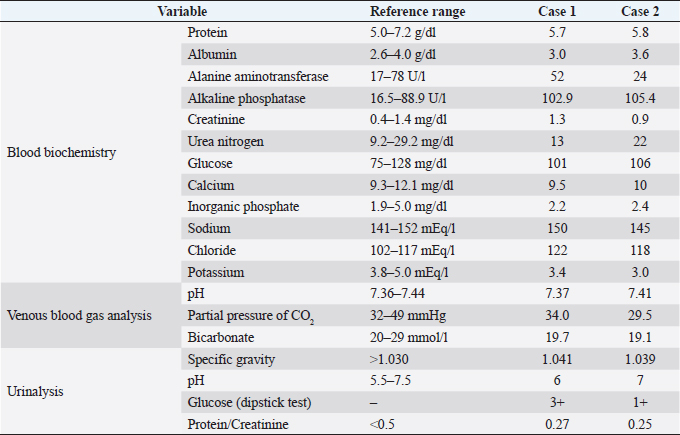
AbstractBackground: Fanconi syndrome (FS) is defined as multiple defects of the proximal tubules and is diagnosed by clinical symptoms. However, in dogs with FS, the damage in the proximal tubules that is responsible for the clinical symptoms has not been evaluated. Among FS cases, tubular damage in acquired FS is reversible following the elimination of a causative factor. Liver-type fatty acid-binding protein (L-FABP) is a biomarker of tubular damage in various animals including dogs. Urinary L-FABP measurement may be useful for the diagnosis and follow-up evaluation in canine FS. Case Description: At the first visit, two Toy Poodles that had no remarkable findings on physical examination presented with glycosuria without hyperglycemia, hypokalemia, hyperchloremia, increased levels of plasma alkaline phosphatase, and metabolic acidosis. Considering all the factors involved, the dogs were clinically diagnosed with acquired FS. The owner reported that they routinely fed the dog with chicken jerky, a recently considered cause of acquired FS. Following the withdrawal of the jerky, abnormalities including glycosuria improved in both dogs. Moreover, urinary L-FABP levels, which were high at diagnosis, presented a decreasing trend during the follow-up. However, in one dog, the elevated urinary L-FABP level did not return to normal. Conclusion: Although the clinical symptoms of acquired FS in dogs could be improved by the elimination of a causative factor, the severity of tubular damage described by urinary L-FABP may not be necessarily linked to the degree of functional deterioration. Therefore, the evaluation of proximal tubular damage by L-FABP may be of clinical value during the follow-up of acquired FS in canines. Keywords: Acquired Fanconi syndrome, Dog, Urinary L-FABP. IntroductionFanconi syndrome (FS) is defined by multiple defects of the proximal tubules, which cause impairment in the reabsorption of molecules, such as glucose, amino acids, bicarbonate, phosphate, and other electrolytes. FS in dogs, which has been well documented as inherited (such as Basenjis) (Noonan and Kay, 1990), is mostly an acquired state associated with exposure to heavy metals and drugs (Bergeron et al., 1995), urinary infections (Green et al., 2006), and certain diseases such as primary hypoparathyroidism (Freeman et al., 1994) and copper-associated hepatopathy (Langlois et al., 2013). Recently, chicken jerky treats produced in China and/or containing Chinese ingredients has well documented to cause acquired FS in dogs, (Thompson et al., 2013; Igase et al., 2015; Bates et al., 2016; Yabuki et al., 2017). Although FS in dogs is diagnosed based on its clinical symptoms such as glycosuria with euglycemia, generalized aminoaciduria, and renal tubular acidosis, the damage in proximal tubules that is responsible for the clinical symptoms has not been evaluated. Some dogs with acquired FS have reversible renal damage following the elimination of a causative factor. The extent of tubular injury in dogs with FS is currently assessed by the abnormalities resulting from the injury, such as diabetes, hypokalemia, and metabolic acidosis. A more sensitive marker of the degree of tubular damage might be required for a follow-up assessment of the reversible renal damage. Renal biopsy is a method of proving tissue damage to the kidney, but it is not commonly performed because of its invasive nature and risk of anesthesia. Liver-type fatty acid-binding protein (L-FABP) is a 14-kDa protein found in the liver and kidney in various animals including dogs (Bass et al., 1989; Su et al., 2004; Furuhashi and Hotamisligil, 2008; Takashima et al., 2021). In human kidneys, L-FABP is found in the cytoplasm of proximal tubular cells (Maatman et al., 1992; Furuhashi and Hotamisligil, 2008), and it is rapidly released into the tubular lumen in response to ischemia or oxidative stress (Kamijo et al., 2004; Yokoyama et al., 2009). Our previous study in dogs demonstrated that patients with acute kidney injury and chronic kidney disease exhibited a high urinary L-FABP level compared with healthy dogs, and urinary L-FABP had a positive correlation with urinary protein (protein/creatinine ratio) in evoking tubular damage (Takashima et al., 2021). Therefore, in dogs, urinary L-FABP may be used to evaluate tubular damage in place of renal pathological examination. This case series aimed to evaluate the severity of tubular damage through urinary L-FABP measurement in the diagnosis and follow-up assessment of acquired FS. We hypothesized that urinary L-FABP levels are elevated in dogs with acquired FS and have a high value as a clinical marker for the diagnosis and monitoring of FS. Case DetailsCase 1 was a 9-year-old spayed female Toy Poodle, weighing 5.3 kg (BCS 5/9). Case 2 was a 1-year-old spayed female Toy Poodle, weighing 3.4 kg (BCS 5/9). These dogs visited the Gifu University Animal Medical Center with a referral from a primary care clinic because of glycosuria without hyperglycemia. At the first visit, both dogs had no remarkable findings on physical examination. Selected laboratory results at the first visit are presented in Table 1. In both cases, abnormal results of routine blood tests included hypokalemia, hyperchloremia, and a moderate increase in plasma alkaline phosphatase. Other routine test results including glucose were all within the normal reference ranges. In the venous blood gas analysis in both cases, the pH was in the normal range, but the result of low bicarbonate concentration and low partial pressure of CO2 suggested minor metabolic acidosis and compensatory respiratory alkalosis, respectively. In the urinalysis of both cases, dipstick testing revealed only glycosuria (although there are some differences), but the specific gravity was within the normal range, and urinary sediments were undetectable by the microscopic test. In both cases, the urinary protein/creatinine ratio was within the normal range, and the urine culture was negative for bacterial growth. Moreover, abnormalities in nephrology and urology on imaging tests including ultrasonography and radiography were not confirmed. By considering the test results at the first visit, FS was suspected in both cases. In the medical interview, the owners reported that their dogs were routinely addicted to chicken jerky containing Chinese ingredients, had not been exposed to any possible causes of acquired FS other than pet jerky treats (no exposure to heavy metals and several drugs), and had not experienced other illnesses in the past. Considering all the factors involved, both dogs were clinically diagnosed with acquired FS due to the ingestion of chicken jerky treats. However, generalized aminoaciduria analysis to support the diagnosis of FS was not performed from the lack of any inspection companies. Thus, on the first visit, the owners were instructed to completely withdraw chicken jerky from the diet. At the return visit, glycosuria was relieved on day 71 in case 1 and day 22 in case 2. Up until the last follow-up, both cases were found to be in a good condition without glycosuria. Table 1. Selected laboratory results in Case 1 and Case 2 at the first visit.
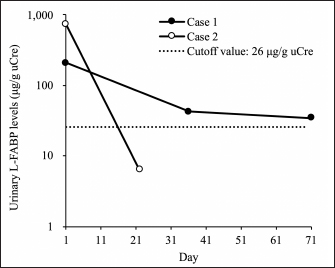
The urinary L-FABP was evaluated at the first presentation and follow-up examination (case 1 on days 1, 36, and 71; case 2 on days 1 and 22). The urinary L-FABP level was measured using a commercial two-step sandwich enzyme-linked immunosorbent assay kit (Canine L-FABP ELISA HS kit, CMIC Holdings, Tokyo, Japan) according to our previous study (Takashima et al., 2021). Urinary L-FABP levels were normal relative to urinary creatinine (uCre) levels to prevent variations caused by the urinary volume. Then, they were expressed as urinary L-FABP (μg/g uCre). The urinary L-FABP values in the two cases at the first visit were higher than the cutoff value for detecting renal disease in our previous study (26 μg/g uCre) (Fig. 1) (Takashima et al., 2021). In case 1, the urinary L-FABP levels during the follow-up declined over time, but had not been below the cutoff value until the final examination day (Fig. 1). In case 2, the urinary L-FABP level at follow-up examination (day 22) was below the cutoff value (Fig. 1). DiscussionThe two cases presented herein were clinically diagnosed with FS based on the presence of glycosuria with euglycemia, hypokalemia, and metabolic acidosis. Clinical symptoms in FS are caused by proximal tubular damage which has been usually evaluated by renal pathological examination. In human L-FABP chromosomal transgenic mouse models, tubulointerstitial damage increased the expression of L-FABP in the proximal tubules and the urinary excretion of L-FABP (Kamijo-Ikemori et al., 2011; Ichikawa et al., 2015). Previous human reports have demonstrated that the severity of proximal tubular damage was related to urinary L-FABP levels (Kamijo et al., 2004; Yokoyama et al., 2009). The presented cases demonstrated that urinary L-FABP levels were higher than the cutoff value of our previous study (Takashima et al., 2021) on the first visit, which suggested tubular damage. In dogs with FS, urinary L-FABP may be an indirect marker used to evaluate tubular damage instead of renal pathological examination.
Fig. 1. Urinary L-FABP in dogs with acquired FS. At the first visit, the urinary L-FABP levels in two cases were higher than the cutoff value for detecting renal disease in our previous study (dash line: 26 μg/g uCre). In case 1, the urinary L-FABP level during the follow-up decline over time, but it is not below the cutoff value at follow-up examination (days 36 and 71) (closed circle). In case 2, the urinary L-FABP level at the follow-up examination (day 22) is below the cutoff value (open circle). After instructing to completely withdraw chicken jerky treats in both cases, abnormalities including glycosuria, hypokalemia, hyperchloremia, and metabolic acidosis were improved. Therefore, in these cases, acquired FS might be caused by chicken jerky treats containing Chinese ingredients as reported previously (Thompson et al., 2013; Igase et al., 2015; Bates et al., 2016; Yabuki et al., 2017). In both cases, urinary L-FABP levels declined over time during the follow-up period. Therefore, urinary L-FABP might describe the progressive amelioration of the proximal tubular damage. However, in case 1, despite the complete disappearance of glucosuria, the urinary L-FABP level on day 71 was still higher than the cutoff value in our previous study (Takashima et al., 2021). In case 1, the tubular damage might not have been fully improved on day 71, although the actual state of damage to the proximal tubules was unknown because pathology with renal biopsy was not performed. Therefore, in canine FS, functional recovery of proximal tubules may be achieved even if the tissues are not completely repaired, and the degree of proximal tubular dysfunction may not necessarily be linked to the severity of tissue damage. A human report of critically ill patients with acute kidney injury demonstrated that a low urinary L-FABP level was an independent prognostic factor for weaning from renal replacement therapy (Pan et al., 2022). Also, during follow-up of dogs with FS, urinary L-FABP may be a useful clinical marker to determine remission in conjunction with tubular function tests. As anticipated, the urinary L-FABP levels of dogs with acquired FS were high at diagnosis, with a decreasing trend during follow-up, which might be changed to reflect tissue damage in the proximal tubule. Although the clinical symptoms of acquired FS could be improved by the elimination of causative factors, the severity of tubular damage described by urinary L-FABP may not be necessarily linked to the degree of functional deterioration. Therefore, the evaluation of proximal tubular damage by L-FABP may be of clinical value during the follow-up of acquired FS in canines. Conflict of interestKeiichi Ohata and Tsuyoshi Oikawa are the senior scientists of CMIC Holdings Co., Ltd. (Tokyo, Japan), a company that produces ELISA kits with high sensitivity for L-FABP analysis. They were responsible for validation analyses and measurement of an ELISA. No other potential conflicts of interest relevant to this article are reported. ReferencesBass, N.M., Barker, M.E., Manning, J.A., Jones, A.L. and Ockner, R.K. 1989. Acinar heterogeneity of fatty acid binding protein expression in the livers of male, female and clofibrate-treated rats. Hepatology 9, 12–21. Bates, N., Sharman, M., Lam, A., Kent, A., Walker, D., Smith, V. and Carmichael, N. 2016. Reporting cases of Fanconi syndrome in dogs in the UK. Vet. Rec. 178, 510. Bergeron, M., Gougoux, A. and Vinay, P. 1995. The renal Fanconi syndrome. In Metabolic and molecular basis of inherited disease. Eds., Sciver, C.R., Beaudet, A.L., Sly, W.S. and Valle, D. New York, NY: McGraw-Hill, pp: 2211–2233. Freeman, L.M., Breitschwerdt, E.B., Keene, B.W. and Hansen, B. 1994. Fanconi’s syndrome in a dog with primary hypoparathyroidism. J. Vet. Intern. Med. 8, 349–354. Furuhashi, M. and Hotamisligil, G.S. 2008. Fatty acid-binding proteins: role in metabolic diseases and potential as drug targets. Nat. Rev. Drug. Discov. 7, 489–503. Green, C.E., Sykes, J.E., Brown, C.A. and Hartman, K. 2006. Leptospirosis. In Infectious diseases of the dog and cat. Ed., Green, C.E. St. Louis, MO: Elsevier, pp: 402–417. Ichikawa, D., Kamijo-ikemori, A., Sugaya, T., Shibagaki, Y., Yasuda, T., Hoshino, S., Katayama, K., Igarashi-Migitaka, J., Hirata, K. and Kimura, K. 2015. Human liver-type fatty acid–binding protein protects against tubulointerstitial injury in aldosterone-induced renal injury. Am. J. Physiol. Renal. Physiol. 308, F114–F121. Igase, M., Baba, K., Shimokawa Miyama, T., Noguchi, S., Mizuno, T. and Okuda, M. 2015. Acquired Fanconi syndrome in a dog exposed to jerky treats in Japan. J. Vet. Med. Sci. 77, 1507–1510. Kamijo, A., Sugaya, T., Hikawa, A., Okada, M., Okumura, F., Yamanouchi, M., Honda, A., Okabe, M., Fujino, T., Hirata, Y., Omata, M., Kaneko, R., Fujii, H., Fukamizu, A. and Kimura, K. 2004. Urinary excretion of fatty acid-binding protein reflects stress overload on the proximal tubules. Am. J. Pathol. 165, 1243–1255. Kamijo-Ikemori, A., Sugaya, T., Matsui, K., Yokoyama, T. and Kimura, K. 2011. Roles of human liver type fatty acid binding protein in kidney disease clarified using hL-FABP chromosomal transgenic mice. Nephrology 16, 539–544. Langlois, D.K., Smedley, R.C., Schall, W.D and Kruger, J.M. 2013. Acquired proximal renal tubular dysfunction in 9 Labrador retrievers with copper-associated hepatitis (2006-2012). J. Vet. Intern. Med. 27, 491–499. Maatman, R.G., van de Westerlo, E.M., van Kuppevelt, T.H. and Veerkamp, J.H. 1992. Molecular identification of the liver- and the heart-type fatty acid-binding proteins in human and rat kidney. Use of the reverse transcriptase polymerase chain reaction. Biochem. J. 288, 285–290. Noonan, C.H. and Kay, J.M. 1990. Prevalence and geographic distribution of Fanconi syndrome in Basenjis in the United States. J. Am. Vet. Med. Assoc. 197, 345–349. Pan, H.C., Huang, T.T., Huang, C.T., Sun, C.Y., Chen, Y.M. and Wu, V.C. 2022. Urinary biomarkers can predict weaning from acute dialysis therapy in critically ill patients. Arch. Pathol. Lab. Med. 146(11), 1353–1363; doi: 10.5858/arpa.2021-0411-OA. Su, A.I., Wiltshire, T., Batalov, S., Lapp, H., Ching, K.A., Block, D., Zhang, J., Soden, R., Hayakawa, M., Kreiman, G., Cooke, M.P., Walker, J.R. and Hogenesch, J.B. 2004. A gene atlas of the mouse and human protein-encoding transcriptomes. Proc. Natl. Acad. Sci. U. S. A. 101, 6062–6067. Takashima, S., Nagamori, Y., Ohata, K., Oikawa, T., Sugaya, T., Kobatake, Y. and Nishii, N. 2021. Clinical evaluation of urinary liver-type fatty acid-binding protein for the diagnosis of renal diseases in dogs. J. Vet. Med. Sci. 83, 1465–1471. Thompson, M.F., Fleeman, L.M., Kessell, A.E., Steenhard, L.A. and Foster, S.F. 2013. Acquired proximal renal tubulopathy in dogs exposed to a common dried chicken treat: retrospective study of 108 cases (2007-2009). Aust. Vet. J. 91, 368–373. Yabuki, A., Iwanaga, T., Giger, U., Sawa, M., Kohyama, M. and Yamato, O. 2017. Acquired Fanconi syndrome in two dogs following long-term consumption of pet jerky treats in Japan: case report. J. Vet. Med. Sci. 79, 818–821. Yokoyama, T., Kamijo-Ikemori, A., Sugaya, T., Hoshino, S., Yasuda, T. and Kimura, K. 2009. Urinary excretion of liver type fatty acid binding protein accurately reflects the degree of tubulointerstitial damage. Am. J. Pathol. 174, 2096–2106. | ||
| How to Cite this Article |
| Pubmed Style Takashima S, Nasu T, Ohata K, Oikawa T, Sugaya T, Kobatake Y, Shibata S, Nishii N. Urinary liver-type fatty acid-binding protein in two dogs with acquired Fanconi syndrome: A case report. Open Vet J. 2022; 12(6): 864-867. doi:10.5455/OVJ.2022.v12.i6.12 Web Style Takashima S, Nasu T, Ohata K, Oikawa T, Sugaya T, Kobatake Y, Shibata S, Nishii N. Urinary liver-type fatty acid-binding protein in two dogs with acquired Fanconi syndrome: A case report. https://www.openveterinaryjournal.com/?mno=81078 [Access: July 11, 2025]. doi:10.5455/OVJ.2022.v12.i6.12 AMA (American Medical Association) Style Takashima S, Nasu T, Ohata K, Oikawa T, Sugaya T, Kobatake Y, Shibata S, Nishii N. Urinary liver-type fatty acid-binding protein in two dogs with acquired Fanconi syndrome: A case report. Open Vet J. 2022; 12(6): 864-867. doi:10.5455/OVJ.2022.v12.i6.12 Vancouver/ICMJE Style Takashima S, Nasu T, Ohata K, Oikawa T, Sugaya T, Kobatake Y, Shibata S, Nishii N. Urinary liver-type fatty acid-binding protein in two dogs with acquired Fanconi syndrome: A case report. Open Vet J. (2022), [cited July 11, 2025]; 12(6): 864-867. doi:10.5455/OVJ.2022.v12.i6.12 Harvard Style Takashima, S., Nasu, . T., Ohata, . K., Oikawa, . T., Sugaya, . T., Kobatake, . Y., Shibata, . S. & Nishii, . N. (2022) Urinary liver-type fatty acid-binding protein in two dogs with acquired Fanconi syndrome: A case report. Open Vet J, 12 (6), 864-867. doi:10.5455/OVJ.2022.v12.i6.12 Turabian Style Takashima, Satoshi, Tomomi Nasu, Keiichi Ohata, Tsuyoshi Oikawa, Takeshi Sugaya, Yui Kobatake, Sanae Shibata, and Naohito Nishii. 2022. Urinary liver-type fatty acid-binding protein in two dogs with acquired Fanconi syndrome: A case report. Open Veterinary Journal, 12 (6), 864-867. doi:10.5455/OVJ.2022.v12.i6.12 Chicago Style Takashima, Satoshi, Tomomi Nasu, Keiichi Ohata, Tsuyoshi Oikawa, Takeshi Sugaya, Yui Kobatake, Sanae Shibata, and Naohito Nishii. "Urinary liver-type fatty acid-binding protein in two dogs with acquired Fanconi syndrome: A case report." Open Veterinary Journal 12 (2022), 864-867. doi:10.5455/OVJ.2022.v12.i6.12 MLA (The Modern Language Association) Style Takashima, Satoshi, Tomomi Nasu, Keiichi Ohata, Tsuyoshi Oikawa, Takeshi Sugaya, Yui Kobatake, Sanae Shibata, and Naohito Nishii. "Urinary liver-type fatty acid-binding protein in two dogs with acquired Fanconi syndrome: A case report." Open Veterinary Journal 12.6 (2022), 864-867. Print. doi:10.5455/OVJ.2022.v12.i6.12 APA (American Psychological Association) Style Takashima, S., Nasu, . T., Ohata, . K., Oikawa, . T., Sugaya, . T., Kobatake, . Y., Shibata, . S. & Nishii, . N. (2022) Urinary liver-type fatty acid-binding protein in two dogs with acquired Fanconi syndrome: A case report. Open Veterinary Journal, 12 (6), 864-867. doi:10.5455/OVJ.2022.v12.i6.12 |