| Research Article | ||
Open Vet J. 2023; 13(5): 501-509 Open Veterinary Journal, (2023), Vol. 13(5): 501–509 Original Research Comparison of cranial versus medial minimally invasive plate osteosynthesis applications for the stabilization of simulated radius and ulna fractures in dog cadaversXiaoXiao Jade Lederer and Daniel Dean Lewis*Department of Small Animal Clinical Sciences, College of Veterinary Medicine, University of Florida, Gainesville, FL 32608, USA *Corresponding Author: Daniel D. Lewis. Department of Small Animal Clinical Sciences, College of Veterinary Medicine, University of Florida, Gainesville, FL 32608, USA. Email: lewisda [at] ufl.edu Submitted: 21/02/2023 Accepted: 03/04/2023 Published: 01/05/2023 © 2023 Open Veterinary Journal
AbstractBackground: Minimally invasive plate osteosynthesis (MIPO) is an emerging fracture management modality in small animal orthopedics. Although cranial plate application has been consistently advocated when performing radial MIPO, medial plating affords several purported advantages including improved screw purchase through the wider medial-to-lateral dimension of the radius, the potential to use smaller plates allowing more screws per unit length, and avoidance of extensor tendons which can complicate cranial plate placement in distal diaphyseal or metaphyseal fractures. Aim: To compare cranial versus medial MIPO applications for the stabilization of diaphyseal radius and ulna fractures in dog cadavers. Methods: Simulated bilateral antebrachial fractures were stabilized with cranial MIPO on one forelimb and medial MIPO on the contralateral limb, facilitated by a two-ring circular fixator construct. Procedure times and ease, number of fluoroscopic images obtained, and post-procedural frontal and sagittal alignment and radial length were compared between plating groups. The ease of construct placement, fracture reduction, radial approach, and plate application, were subjectively scored 1–5 for each procedure. Paired t-tests were performed to identify significant differences (p < 0.05) between the two plating groups. Results: There was no difference in total or incremental procedural times, subjective ease scores, or the number of fluoroscopic images obtained between plating groups. Both plating groups had comparable post-procedural frontal and sagittal plane alignment. There was a significant difference between plating groups for final radial length (p =0.004) and change in radial length compared to the intact radii, (p =0.002). Medial-plated radii measured longer than cranial-plated radii. Conclusion: The only outcome measure significantly different between plating groups was the post-procedural radial length. The change in length compared to intact radii was <1%, regardless of the plating group, and unlikely to be clinically relevant. Keywords: Fracture, MIPO, Orthopedic, Radius, Surgery. IntroductionOpen plate stabilization of radial fractures conventionally involves cranial plate placement (Harrison, 1984; Johnson, 2003); however, some surgeons have advocated applying the plate to the medial surface of the radius (Sardinas and Montavon, 1997). Medial plating affords several purported advantages including improved screw purchase through the wider dimension of the elliptical radius increasing resistance to screw pullout, the potential to use a plate that accepts smaller diameter screws allowing more screws per unit length, and avoidance of interference from the extensor tendons which can complicate cranial plate placement in distal diaphyseal or metaphyseal radial fractures (Sardinas and Montavon, 1997). Biomechanical studies comparing osteotomized radii stabilized with a cranially-placed 3.5 mm plate to a medially-applied 2.7 mm plate reported comparable axial stiffness between constructs (Wallace et al., 1992). Positioning the plate on the medial radius distributes craniocaudal bending forces along the plate’s width, offering greater biomechanical stiffness than cranial plating, where the comparatively thinner dimension (thickness) of the plate must withstand craniocaudal bending forces (Wallace et al., 1992; Uhl et al., 2013). Minimally invasive plate osteosynthesis (MIPO) is an emerging fracture management modality in small animal orthopedics (Schmökel et al., 2003, 2007; Hudson et al., 2009; Pozzi et al., 2021). Several case series have reported positive clinical and radiographic results of MIPO applications for the stabilization of antebrachial fractures in dogs (Witsberger et al., 2010; Pozzi et al., 2012, 2013; Townsend and Lewis, 2018). Transient application of an external fixator has proven highly advantageous to facilitate indirect reduction and alignment, prior to plate placement when performing MIPO stabilization of antebrachial fractures (Hudson et al., 2009, 2012; Pozzi et al., 2012, 2013; Gilbert et al., 2017; Townsend and Lewis, 2018). Cranial plate placement has been consistently advocated when performing radial MIPO applications (Hudson et al., 2009, 2012; Pozzi and Lewis, 2009; Pozzi et al., 2012, 2013, 2021; Gilbert et al., 2017; Townsend and Lewis, 2018) and was used uniformly in reported case series documenting results with MIPO antebrachial fracture stabilization (Witsberger et al., 2010; Pozzi et al., 2012; Townsend and Lewis, 2018). Medial plate application might prove easier when performing MIPO stabilization of the radius, particularly when stabilizing distal radial fractures, as the medial surface of the radius can be readily exposed without interference from the antebrachial extensor tendons. The purpose of this cadaveric study was to evaluate the feasibility of medial plating when performing MIPO of radial fractures and compare surgical time, perceived ease of performance as well as post-stabilization alignment of simulated comminuted radius and ulna fractures to cranial MIPO applications. We hypothesized both plate applications would yield equivalent fracture alignment, but medial plating would be easier to perform, decreasing procedural times. Materials and MethodsCadaver procurement and preparationMixed breed dogs euthanized for reasons unassociated with the study were obtained. All cadavers had been previously frozen but were thawed and stored in a cooler for a minimum of 3 days prior to use. Bilateral orthogonal radiographs were obtained (Vet-ray, Sedecal, Niles, IL) of the antebrachium and manus to ensure normalcy and allow for preemptive measurements of antebrachial morphology. A 25-mm diameter sphere was placed adjacent to the radius in all images to allow for image calibration. Image analysis was performed on a dedicated computer using DICOM viewing software (MergePACS, Merative, Ann Arbor, MI). Angle measurements were made using a Chrome browser protractor extension (“Protractor”, Ben Burlingham) and lengths were calculated in an orthopedic planning program (vPOP PRO, VETSOS Education Ltd., Ojai, CA). Joint reference lines, anatomic axes, radial joint angles, and frontal and sagittal plane alignments were established as described by Fox and Tomlinson (2018). Procurvatum was quantified as the acute angle (theta) created from the intersection of the proximal and distal radial sagittal anatomic axes. The radial length was measured on sagittal view images and defined as the distance between the caudal margins of the radial head and of the distal radial articular surface (Fig. 1). Cranial or medial radial plating was performed by MIPO on the contralateral forelimbs in each cadaver. The limb undergoing medial versus lateral plating alternated between cadavers so that an equal number of each application was performed on the right and left thoracic limbs. A 2-ring circular fixator construct (IMEX Veterinary, Inc. Longview, TX) was used in all cadavers to facilitate the MIPO application. Two 84-mm complete rings were articulated with three threaded connecting rods and secured in place using 6-mm hex nuts. The threaded connecting rods were positioned asymmetrically about the circumference of the ring such that 9, 7, and 5 empty holes were spaced between the rods; 150-mm rods were used in smaller cadavers and 255-mm rods were used in larger cadavers. Both forelimbs were shaved from the shoulder to the digits, consistent with standard pre-procedural preparation for antebrachial fracture stabilization. The cadavers were placed in dorsal recumbency. A limited lateral approach was made exposing the mid-diaphyseal region of the radius and ulna and a simulated comminuted mid-diaphyseal radial fracture and a simulated mid-diaphyseal segmental ulnar fracture were made using a battery-operated handpiece with an oscillating saw attachment (DePuy Synthes, Raynham, MA) and 5-mm saw blade (Gilbert et al., 2017). Displacement and malalignment of the fractured radius were induced by manipulating the antebrachium through the fracture. Fluoroscopy (Ziehm Imaging, Orlando, FL) was used to confirm the location and completeness of the osteotomies. The approach was closed in a single layer using 3–0 nylon in a Ford interlocking pattern. Application of the fixator construct and fracture alignment and reductionThe senior author served as the primary surgeon during all MIPO applications, assisted by the first author. The radiocarpal articulation was identified with an 18-gauge needle. The same battery-operated handpiece with a wire and pin collet attachment was used to place a 1.6-mm Kirschner wire in the proximal radial metaphysis. For limbs undergoing cranial plating, the proximal Kirschner wire was placed lateral-to-medial. The wire was oriented perpendicular to the frontal plane proximal anatomic axis with an equal length of the wire protruding from both sides of the antebrachium. The preassembled 2-ring fixator construct was placed over the limb, with the largest window positioned over the cranial aspect of the antebrachium where the anticipated plate insertional incisions would be made. The Kirschner wire was attached to the proximal ring using wire fixation bolts. A second medial-to-lateral Kirschner wire was placed through the distal radial metaphysis, perpendicular to the distal radial frontal plane anatomic axis, and adjacent to the radiocarpal articulation. Traction was applied to the distal ring to bring the ring in contact with the distal Kirschner wire. The Kirschner wire was attached to the distal ring using wire fixation bolts. The elbow and carpus were flexed and the distal limb was viewed from the caudal surface of the antebrachium to ensure that rotational alignment was acceptable. If rotational malalignment was present, the fixation bolts securing the distal wire were removed and the position of the wire was adjusted about the circumference of the ring until the elbow and the carpus flexed and extended through the same sagittal plane before re-securing the wire to the distal ring.
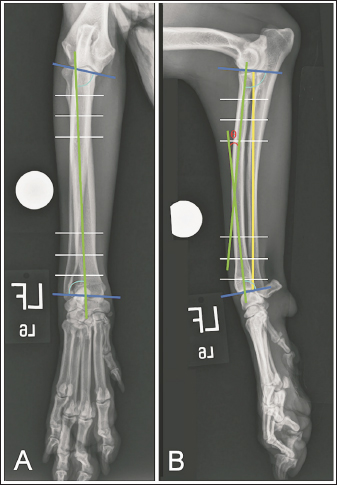
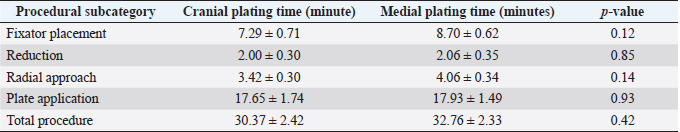
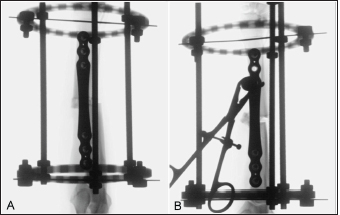
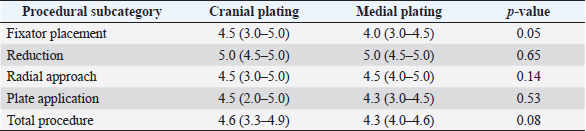
Fig. 1. Orthogonal radiographic images illustrating how joint reference lines (dark blue) and anatomic axes (green) were established to define the proximal and distal anatomic radial joint angles (light blue) on intact limbs. White lines are paired with 10% (outermost lines), 20% (middle lines), and 30% (innermost lines) markers along the length of the proximal and distal radius used to define anatomic axes. Radial length (yellow) was measured as the distance between the caudal margins of the articular surface of the radial head and of the distal radial articular surface. Theta (θ) was measured as the acute angle created at the intersection of anatomic axes. Distraction was performed by applying traction to the distal ring as the nuts located proximal to the distal ring were manually rotated with a finger. The nuts were advanced along the threaded rods until the nuts contacted the proximal surface of the distal ring and alignment and reduction were considered acceptable based on palpation and gross appearance. Fluoroscopy was used to critique alignment and reduction in both the frontal and sagittal planes. If translation existed in the frontal plane, alignment was improved by translating one or both primary fracture segments in a medial or lateral direction along the implanted Kirschner wires. The process was similar for limbs undergoing medial plating, but the Kirschner wires were placed cranial-to-caudal; one wire was placed subjacent to the radial head and the second wire was placed in the distal radial metaphysis. The largest window of the fixator was positioned over the medial surface of the antebrachium. Cranial or caudal translation of one or both of the major fracture segments along the implanted Kirschner wires was used when needed, to improve sagittal plane alignment. Plate placementSix-hole 3.5-mm conical coupling locking plates ranging in length from 81- to 139-mm (Fixin, Intrauma S.p.A., Rivoli, Italy) were pre-contoured using the sagittal radiographic image of the intact radius for cranial plate applications and the frontal plane image of the intact radius for medial plate applications. Two 3-cm craniomedial plate insertional incisions were made. The location of these incisions was determined by positioning an appropriate-length plate over the antebrachium. The first incision was made in the region of the distal radial metaphysis, determined by the anticipated position of the distal three holes of the plate. The tendon of insertion of the abductor pollicis longus muscle and extensor carpi radialis were identified and retracted craniodistal to allow cranial plate placement. A Freer periosteal elevator was used to expose the distal radius. The second plate insertional incision was made over the proximomedial margin of the radial diaphysis, with the location determined by the anticipated position of the proximal holes of the plate. Metzenbaum scissors were utilized to create an epiperiosteal tunnel between the incisions. The pre-contoured plate was inserted into the distal plate insertional incision and advanced along the cranial surface of the radius through the epiperiosteal tunnel. The plate was initially secured to the proximal and distal radial fracture segments with two 1.0-mm Kirschner wires placed in the designated wire holes in the plate, through the respective insertional incisions. Plate placement, as well as fracture alignment and reduction, were assessed by palpation and verified by fluoroscopy after a screw was placed both proximally and distally. Adjustments were performed, if required, and once alignment and reduction were deemed suitable, two additional screws were placed both proximally and distally. The fixator was removed. Final alignment and reduction as well as satisfactory plate placement were assessed using fluoroscopy, and if needed, final adjustments were made. The surgical site was closed routinely. Medial plating was performed similarly although the distal plate insertional incision was positioned directly medial, and the pronator teres muscle was elevated more extensively through the proximal plate incision to expose the medial surface of the proximal radius. The number of fluoroscopic images taken, procedure times, and Likert scores characterizing the ease of construct placement, fracture distraction and alignment, developing the radial approach, and plate placement, were compared between plating groups. Outcome measuresPost-procedural orthogonal antebrachial radiographs of both antebrachia were obtained. Post-procedural measurements for radial length, frontal and sagittal alignment, and pro- or recurvatum were compared between plating groups. Post-procedural frontal plane alignment was determined by drawing proximal and distal radial joint reference lines and transferring the pre-procedural proximal and distal radial joint angles to the post-procedural frontal images to define the proximal and distal frontal plane anatomic axes. Angular deviation at the intersection of these axes defined the varus or valgus radial alignment (Gilbert et al., 2017). Post-procedural sagittal plane alignment was determined by drawing proximal and distal joint reference lines and transferring the pre-procedural sagittal joint angles to the post-procedural sagittal images to define proximal and distal sagittal anatomic axes. Post-procedural theta was subtracted from pre-procedural theta to quantify the respective increase or decrease in procurvatum. Post-procedural alignment was also subjectively characterized as near-anatomic, acceptable, or unacceptable according to criteria previously described (Johner and Wruhs, 1983; Rubinstein et al., 1992; Puloski et al., 2004; Johnson et al., 2022). Statistical analysisAll data sets were tested for normality of distribution with the Shapiro–Wilks test. Excluding Likert scores, all data sets were normally distributed and reported as mean ± SEM and paired t-tests were performed to compare: overall procedure time, time of procedural subcategories previously defined, and changes in frontal and sagittal angulation, as well as radial length following plating, between plating groups. The overall and procedural sub-categorical subjective ease scores were compared between plating groups with the Mann-Whitney U test and reported as median (range). p < 0.05 was considered statistically significant. Ethical approvalThe 10 mixed-breed dog cadavers used in the present study were obtained in accordance with the University of Florida research policies. ResultsThe cadavers weighed between 23 and 41 kg. All intact radii had normal frontal plane conformation with a single anatomic axis. The mean ± SEM for the anatomic medial proximal radial angle (aMPRA) and anatomic lateral distal radial angle (aLDRA) of intact radii was 80.8° ± 0.7° and 86.1° ± 0.7°, respectively, and did not differ between plating groups (p =0.77 and 0.67, for aMPRA and aLDRA, respectively). All intact radii had some degree of natural procurvatum. Sagittal plane angulation was comparable between intact radii (procurvatum mean ± SEM: 13.6° ± 0.7°) and did not differ between plating groups (p =0.96). The mean ± SEM anatomic caudal proximal joint angle (aCdPRA) and anatomic caudal distal radial angle (aCdDRA) were 86.9° ± 0.7° and 81.1° ± 0.8°, respectively, and did not differ between plating groups (p =1 and 0.7 for aCdPRA and aCdDRA, respectively). Length of intact radii ranged from 116.3 to 172.5 mm (mean ± SEM: 147.9 ± 3.7 mm) and did not differ between plating groups (p =0.12). The total procedure time as well as incremental times for the subcategories of fixator placement, reduction, radial approach, and plate application did not differ between the cranial and medial plating groups (Table 1). Placement of the proximal Kirschner wire was more cumbersome than distal wire placement in both plating groups. Proximal cranial-to-caudal Kirschner wire placement was also more challenging than medial-to-lateral wire placement. Wire obliquity had to be addressed in four limbs in the cranial plating group and five limbs in the medial plating group. Obliquity was addressed by placing flat washers on one or both of the fixation bolts securing the Kirschner wire (n=1 limb in each plating group), attaching the fixation wire on opposite surfaces of the ring (n=1 and 2 in the cranial and medial plating group, respectively), or removing and replacing the wire (n=4 and 3 in the cranial and medial plating group, respectively). Lateral translation of the distal fracture segment along the Kirschner wire was performed to improve frontal plane alignment prior to plating in three limbs in the cranial plating group (Fig. 2). Caudal translation of the distal fracture segment along the Kirschner wire was performed to improve sagittal plane alignment prior to plating in two limbs in the medial plating group (Fig. 3). Obtaining sufficient exposure of the proximal radius to allow for plating required substantial tissue dissection, particularly in larger cadavers in both plating groups. The distal ring interfered with establishing a distal-to-proximal epiperiosteal tunnel in one limb in the cranial plating group, necessitating proximal-to-distal development. Plate orientation was more craniomedial than medial in six limbs in the medial plating group. Bone-holding forceps were used to improve reduction and alignment and to maintain appropriate plate position on the radius during plating in five limbs in the cranial plating group and six limbs in the medial plating group. Alignment was also similarly improved using bone holding forceps following initial plate placement by loosening then retightening or removing and replacing screws in four limbs in both plating groups (Fig. 4). The proximal or distal ring interfered with inserting the locking drill guide into the plate in three limbs in both plating groups. The fixator was removed in these limbs to allow placement of the final proximal or distal screw. Total and incremental procedure subcategory Likert scores assessing ease of performance did not differ between plating groups (Table 2). The number of fluoroscopic images (mean ± SEM: 8.7 ± 0.9 and 9.0 ± 0.8 for cranial and medial plating groups, respectively) obtained during the procedure did not differ between plating groups (p =0.77). Table 1. Subcategory and procedure times. Comparison of subcategory and total procedure times for cranial and medial plating groups. Data are expressed as mean ± SEM. p-value < 0.05 is considered significant.
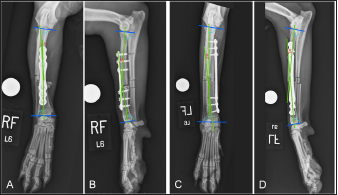
Six plated radii in each plating group had some degree of valgus and four plated radii in each plating group had some degree of varus. Frontal plane alignment of cranially plated radii ranged from 11.1° valgus to 3.5° varus. Frontal plane alignment of medially plated radii ranged from 4° valgus to 12.8° varus. Post-procedural frontal alignment (mean ± SEM: 1.8° ± 1.5° valgus and 1.2° ± 1.6° varus in the cranial and medial plating groups, respectively) did not differ between plating groups (p =0.10). Five radii in the cranial plating group had decreased procurvatum and five had increased procurvatum. Seven radii in the medial plating group had decreased procurvatum while three had increased procurvatum (Fig. 5). Sagittal plane alignment of cranially plated radii ranged from 3.0° to 18.2° of procurvatum. Medially plated radii had 5.2° to 21.4° of procurvatum. Post-procedural sagittal plane alignment (mean ± SEM: 11.5° ± 1.8° and 12.0° ± 1.6° in the cranial and medial plating groups, respectively) did not differ between plating groups (p =0.81). Procurvatum was decreased in both plating groups (mean ± SEM: −2.1° ± 1.5° and −1.7° ± 1.3° in the cranial and medial plating groups, respectively) and there was no difference in the magnitude of change in procurvatum between plating groups (p =0.82). Post-procedural radial length ranged from 117.6 to 171.6 mm in cranially plated radii and from 117.9 to 173.8 in medially plated radii. The post-procedural radial length of cranially plated radii was decreased relative to the intact radii (mean difference ± SEM: −1.06 ± 0.71 mm), while the radial length of medially plated radii was increased relative to the intact radii (mean difference ± SEM: 1.11 ± 0.54 mm). The post-procedural radial length was significantly different between plating groups (p =0.004) along with the change in radial length, compared to intact radii, between plating groups (p =0.002). “Near-anatomic” frontal plane alignment was obtained in eight cranial and nine medial-plated radii. “Near-anatomic” sagittal plane alignment was obtained in six cranial and seven medial-plated radii. Post-procedural radii were considered to have “acceptable” frontal plane alignment in one cranially plated radius. Post-procedural sagittal plane alignment was considered “acceptable” in four cranial and three medial-plated radii. Frontal plane alignment was considered “unacceptable” in one radius in each plating group.
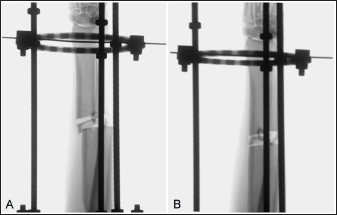
Fig. 2. Fluoroscopic images of a limb assigned to the cranial plating group obtained after application of the circular construct. The Kirschner wires were placed from medial to lateral. Note that the distal fracture segment is medially displaced after the radius and ulna had been distracted out to length (A). Manual pressure was applied to the medial aspect of the distal radial segment to translate the segment laterally along the implanted Kirschner wire to improve frontal plane alignment (B).
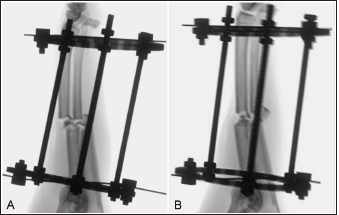
Fig. 3. Fluoroscopic images of a limb assigned to the medial plating group obtained after the application of the circular construct. The Kirschner wires were placed from cranial to caudal. Note that the distal fracture segment is cranially displaced after the radius and ulna had been distracted out to length (A). Manual pressure was applied to the cranial aspect of the distal radial segment to translate the segment caudally along the implanted Kirschner wire to improve sagittal plane alignment (B). DiscussionDescriptions of radial MIPO applications uniformly describe cranial plate placement (Witsberger et al., 2010; Hudson et al., 2012; Pozzi et al., 2013; Gilbert et al., 2017) and are often facilitated by the transient intraoperative application of a circular external fixator construct (Hudson et al., 2012; Pozzi et al., 2013; Gilbert et al., 2017). Medial plating of radial fractures has several purported advantages (Sardina and Montavon, 1997), but to date, there are no reports of medial radial MIPO applications for the stabilization of antebrachial fractures. In this cadaveric study, we compared medial to cranial plate placement for radial MIPO applications and found no difference in procedural time, Likert scores assessing procedural ease, the number of fluoroscopic images obtained, or frontal or sagittal alignment between plating groups.
Fig. 4. Fluoroscopic images of a limb assigned to the cranial plating group. After initial plating, there was valgus angulation of the distal fracture segment (A). The two most-proximal screws engaging the distal radial segment were removed and the distal screw was loosened and bone-holding forceps were applied through the plate insertional incision to improve alignment (B). Screws were subsequently reinserted and the distal screw tightened. Valgus angulation of the distal fracture segment is often induced during open cranial plating of distal radial fractures secondary to the predominance of lateral antebrachial musculature and lateral retraction of the extensor tendons during surgery (Sardinas and Montavon, 1997). In a retrospective clinical study assessing MIPO stabilization of antebrachial fractures with cranially applied plates, Pozzi et al. (2013) reported a mean post-operative frontal plane alignment of 4.7° valgus. Similarly, Gilbert et al. (2017) reported a mean post-procedural frontal plane alignment of 4° valgus in a cadaveric study assessing MIPO stabilization of antebrachial fractures with cranially applied plates. While 6 of the 10 cranial-plated radii in the current study had a valgus alignment, 4 had varus and the absolute mean deviation was only 1.8°; frontal plane alignment was similar in the medial-plated group. We attribute the lack of consistent valgus in cranial plated radii to uniform distraction of the fracture segments afforded by the circular construct and applying the plate beneath the distal extensor tendons without extensive retraction of the extensor tendon. The tendency toward minor varus in medial plated radii was presumed to be secondary to over-contouring the plate in an attempt to conform to distomedial radial morphology. There was a tendency toward procurvatum being slightly reduced in both plating groups. The authors would have expected the application of a linear plate to the medial surface of the radius to have reduced procurvatum to a greater degree than the application of a well-contoured plate to the cranial surface. We suspect the under-contouring of the plates was responsible for the slightly greater decrease in procurvatum in the cranial plating group. The post-procedural radial length was the only outcome measure significantly different between plating groups. Medial-plated radii were longer than pre-procedural intact radii and post-procedural cranial-plated radii, while cranial-plated radii were shorter than pre-procedural intact radii. Factors contributing to these differences are unclear, but the mean discrepancy in length between intact and plated radii in both plating groups was <1% and would presumably have a negligible effect on limb function (Franczuszki et al., 1987; Boston and Skinner, 2018). Table 2. Subcategory and procedure Likert scores. Comparison of subcategory and total procedure Likert scores evaluating ease between cranial and medial plating groups. The Likert scoring system utilized: 1=very difficult, 2=difficult, 3=neither difficult nor easy, 4=easy, 5=very easy. Data are expressed as median (range). p-value < 0.05 is considered significant.
Fig. 5. Orthogonal radiographic images of plated radii illustrating trends in frontal and sagittal plane angulation following cranial (A–B) and medial (C–D) plating. Proximal and distal joint reference lines were drawn and joint reference angles were transferred from the intact radii to the plated radii to establish proximal and distal anatomic axes to determine frontal and sagittal plane malalignment. In the cranial plated radius (A–B) there is slight (1°) valgus angulation (A) and decreased (by 7.7° to 5.2°) procurvatum (B), following plating. In the medial plated radius (C–D) there is slight (3.9°) varus angulation (C) and decreased (by 4.4° to 6.7°) procurvatum (D), following plating. Unanticipated difficulties encountered during medial plating included challenges in placing the proximal Kirschner wire, maintaining medial plate orientation on the radii, needing to elevate the pronator teres muscle, and construct rings interfering with screw placement. Placing fixation wires perpendicular to the relevant anatomic axis is essential to appropriate circular fixator application as well as to avoid creating frontal or sagittal plane angulation (Anderson et al., 2003). Placement of the proximal Kirschner wire during fixator application, particularly wires placed cranial-to-caudal, was challenging because of greater surrounding musculature proximally and wires placed cranial-to-caudal often penetrated both the radius and the ulna. Distal cranial plate application can be cumbersome due to impedance from the distal antebrachial extensor tendons. Medial plating was expected to be easier than cranial plating given a lack of anatomic structures that would impede medial plate application in the distal metaphyseal region; however, Likert scores were comparable between plating groups. The compressed sagittal dimension of the elliptical radius made the medial positioning of the plates challenging, particularly proximally and in smaller cadavers. We used bone-holding forceps to appropriately position the plate in some cadavers; however, final orthogonal radiographs confirmed plates were positioned craniomedial in six medial-plated radii. Loosening and retightening screws allowed small adjustments to be made to improve fracture apposition as well as alignment. The use of bone-holding forceps proved to be advantageous in temporarily stabilizing the bone-plate interface, improving apposition while minimizing cranial displacement of the plate. Greater tissue dissection was required to expose the proximal radius, particularly during medial plate application. Elevation of the pronator teres muscle was subjectively more extensive with medial plating than cranial plating, which could potentially diminish some of the benefits ascribed to MIPO (Baumgaertel et al., 1998; Hudson et al., 2012). Stretch or ⅝ partial rings are typically used when performing cranial MIPO applications. Cranially positioning the open section of incomplete rings allows a full range of motion in the elbow and simplifies the development of the epiperiosteal tunnel and plate application (Hudson et al., 2009, 2012). Orienting the open section of the rings in different locations about the circumference of the limb would have introduced another variable between plating groups, therefor our constructs were made using two complete rings to maintain consistency between plating groups. Medial plate application necessitated positioning a solid section of each ring cranially to secure the cranial-to-caudal placed Kirschner wires to the construct. Alternatively, consideration could be given to placing the Kirschner wires medial-to-lateral in the medial plating group which would allow the use of stretch or ⅝ partial rings. Using rings with an open section positioned cranially might simplify epiperiosteal tunnel development and plate application, but in the senior author’s experience, having the wires positioned orthogonal to the osseous surface of plate application facilitates improved fracture alignment and reduction. Additionally, a medial-to-lateral Kirschner wire could interfere with distal plate placement in medially plated radii, as many clinical fractures involve the distal diaphysis (Milovancev and Ralphs, 2004). The distal ring interfered with establishing the epiperiosteal tunnel in the one limb in the cranial plating group and had to be removed in three limbs in both plating groups to allow for placement of the final proximal or distal screw. Fixator removal did not adversely impact reduction or alignment as four or five screws had already been placed in these limbs. Limitations of this study include the study’s cadaveric nature, the mid-diaphyseal location of the simulated fractures, uniform use of 3.5 mm bone plates, and surgeon bias from a comparative lack of experience with medial MIPO applications. Local soft tissue constraints normally present during clinical fracture stabilization are not present in an acute cadaveric fracture model (Gilbert et al., 2017; Johnson et al., 2022). Distracting the fractured antebrachium out to length was reliably accomplished by applying manual traction to the distal ring. In clinical fractures, resistance is greater and rotation of the nuts on the threaded connecting rods with a wrench is often necessary to obtain sufficient distraction to align and reduce fractures. In this study, we only evaluated the stabilization of mid-diaphyseal fractures. Most radial fractures are located in the distal third of the diaphysis (Milovancev and Ralphs, 2004) and medial plating might prove to be comparatively easier than cranial plating, mainly due to the avoidance of impendence with the distal extensor tendons. We used 3.5 mm plates exclusively in this study to maintain consistency between plating groups. Fixin plates are particularly useful when performing cranial MIPO applications because of the low profile of the plates (Nicetto et al., 2013). The Fixin plates are, however, relatively wide and did not conform well to the medial surface of the radius, particularly proximally. We suspect narrower plates would have been simpler to apply to the medial surface of the radius and the use of a 2.7 mm plate would theoretically offer the ability to place more screws in the distal fracture segment than a 3.5 mm plate (Sardinas and Montavon, 1997; Uhl et al., 2013). The advantageous biomechanical attributes associated with medial plate placement imply that the application of a smaller-sized plate medially might be appropriate. Despite the senior investigator, who performed all of the stabilization procedures in this study, having substantial experience performing cranial MIPO of radial fractures and no prior experience performing medial radial MIPO applications, outcome measures were similar between plating groups. The primary surgeon’s inexperience with medial radial MIPO applications may have negatively impacted proficiency in the medial plating group. Evaluating the ease of this technique through the performance of a single surgeon also lends inherent bias and is a notable limitation of this study. Our results, however, suggest that fixator-assisted medial radial MIPO may have merit and could potentially prove more efficient with increased surgeon experience. Further experimental and clinical studies enrolling surgeons with varying experience with MIPO stabilization are warranted to better evaluate the difficulties and advantages associated with medial MIPO application for stabilizing antebrachial fractures. AcknowledgmentsThis project was supported with funds and implants provided by Intrauma S.p.A., Rivoli, Italy. Additional funding was provided by the Jeff and Jo Godwin Advanced Small Animal Surgical Training and Canine Gait Laboratory. Special thanks to Dr. Mehmet Zeki Yilmaz Deveci for his tremendous assistance with the cadavers during the procedures, Dr. Matthew Johnson for providing helpful references, Debby Sundstrom for creating manuscript figures, and James Colee for reviewing the data and confirming appropriate statistical analysis was performed. Conflict of interestThe authors declare that there is no conflict of interest. Neither author is contractually affiliated with Intrauma S.p.A. Author contributionsLederer X., DVM: contributed to the design of the study, identified suitable cadavers, recorded demographic information, assisted during the procedures, performed radiographic measurements, compiled all data, analyzed data for statistical significance, and drafted and revised the manuscript. Lewis D., DVM, Diplomate ACVS: contributed to the design of the study, performed the procedures, and drafted and revised the manuscript. ReferencesAnderson, G.M., Lewis, D.D., Radasch, R.M., Marcellin-Little, D.J., Degna, M.T. and Cross, A.R. 2003. Circular external skeletal fixation stabilization of antebrachial and crural fractures in 25 dogs. J. Am. Anim. Hosp. Assoc. 39, 479–498. Baumgaertel, F., Buhl, M. and Rahn, B.A. 1998. Fracture healing in biological plate osteosynthesis. Injury 29, C3–C6. Boston, S.E. and Skinner, O.T. 2018. Limb shortening as a strategy for limb sparing treatment of appendicular osteosarcoma of the distal radius in a dog. Vet. Surg. 47, 136–145. Fox, D.B. and Tomlinson, J.L. 2018. Principles of angular limb deformity correction. In Veterinary surgery small animal, 2nd ed. Eds., Johnston, S.A. and Tobias, K.M. St. Louis, MO: Elsevier, pp: 62–764. Franczuszki, D., Chalman, J.A., Butler, H.C., DeBowes, R.M. and Leipold, H. 1987. Postoperative effects of experimental femoral shortening in the mature dog. J. Am. Anim. Hosp. Assoc. 23, 429–437. Gilbert, E.D., Lewis, D.D., Townsend, S. and Kim, S.E. 2017. Comparison of two external fixator systems for fracture reduction during minimally invasive plate osteosynthesis in simulated antebrachial fractures. Vet. Surg. 46, 971–980. Harrison, J.W. 1984. Fractures of the radius and ulna in the dog. In Manual of internal fixation in small animals, 1st ed. Eds., Brinker, W.O., Hohn, R.B. and Prieur, W.D. New York, NY: Springer-Verlag, pp: 144–151. Hudson, C.C., Lewis, D.D. and Pozzi, A. 2012. Minimally invasive plate osteosynthesis in small animals: radius and ulna fractures. Vet. Clin. North. Am. Small. Anim. Pract. 42, 983–vii. Hudson, C.C., Pozzi, A. and Lewis, D.D. 2009. Minimally invasive plate osteosynthesis: applications and techniques in dogs and cats. Vet. Comp. Orthop. Traumatol. 22, 175–182. Johner, R. and Wruhs, O. 1983. Classification of tibial shaft fractures and correlation with results after rigid internal fixation. Clin. Orthop. Relat. Res. 178, 7–25. Johnson, A.L. 2003. Current concepts in fracture reduction. Vet. Comp. Orthop. Traumatol. 16, 59–66. Johnson, M.D., Lewis, D.D., Sutton, W.A., Scheuermann, L.M., De Armond, C.C., Kim, S.E. and Biedrzycki, A.H. 2022. Efficacy of two reduction methods in conjunction with 3-D-printed patient-specific pin guides for aligning simulated comminuted tibial fractures in cadaveric dogs. Am. J. Vet. Res. 83(9), 1-10.. Milovancev, M. and Ralphs, S.C. 2004. Radius/ulna fracture repair. Clin. Tech. Small. Anim. Pract. 19, 128–133. Nicetto, T., Petazzoni, M., Urizzi, A. and Isola, M. 2013. Experiences using the Fixin locking plate system for the stabilization of appendicular fractures in dogs: a clinical and radiographic retrospective assessment. Vet. Comp. Orthop. Traumatol. 26, 61–68. Pozzi, A., Hudson, C.C., Gauthier, C.M. and Lewis, D.D. 2013. Retrospective comparison of minimally invasive plate osteosynthesis and open reduction and internal fixation of radius-ulna fractures in dogs. Vet. Surg. 42, 19–27. Pozzi, A. and Lewis, D.D. 2009. Surgical approaches for minimally invasive plate osteosynthesis in dogs. Vet. Comp. Orthop. Traumatol. 22, 316–320. Pozzi, A., Lewis, D.D., Scheuermann, L.M., Castelli, E. and Longo, F. 2021. A review of minimally invasive fracture stabilization in dogs and cats. Vet. Surg. 50, O5–16. Pozzi, A., Risselada, M. and Winter, M.D. 2012. Assessment of fracture healing after minimally invasive plate osteosynthesis or open reduction and internal fixation of coexisting radius and ulna fractures in dogs via ultrasonography and radiography. J. Am. Vet. Med. Assoc. 241, 744–753. Puloski, S., Romano, C., Buckley, R. and Powell, J. 2004. Rotational malalignment of the tibia following reamed intramedullary nail fixation. J. Orthop. Trauma. 18, 397–402. Rubinstein, R.A., Green, J.M. and Duwelius, P.J. 1992. Intramedullary interlocked tibia nailing: a new technique (preliminary report). J. Orthop. Trauma. 6, 90–95. Sardinas, J.C. and Montavon, P.M. 1997. Use of a medial bone plate for repair of radius and ulna fractures in dogs and cats: a report of 22 cases. Vet. Surg. 26, 108–113. Schmökel, H.G., Hurter, K. and Schawalder, P. 2003. Percutaneous plating of tibial fractures in two dogs. Vet. Comp. Orthop. Traumatol. 16, 191–195. Schmökel, H.G., Stein, S., Radke, H., Hurter, K. and Schawalder, P. 2007. Treatment of tibial fractures with plates using minimally invasive percutaneous osteosynthesis in dogs and cats. J. Small. Anim. Pract. 48, 157–160. Townsend, S. and Lewis, D.D. 2018. Use of the minimally invasive reduction instrumentation system for facilitating alignment and reduction when performing minimally invasive plate osteosynthesis in three dogs. Case. Rep. Vet. Med. 2018, 1-8. Uhl, J.M., Kapatkin, A.S., Garcia, T.C. and Stover, S.M. 2013. Ex vivo biomechanical comparison of a 3.5 mm locking compression plate applied cranially and a 2.7 mm locking compression plate applied medially in a gap model of the distal aspect of the canine radius. Vet. Surg. 42, 840–846. Wallace, M.K., Boudrieau, R.J., Hyodo, K. and Torzilli, P.A. 1992. Mechanical evaluation of three methods of plating distal radial osteotomies. Vet. Surg. 21, 99–106. Witsberger, T.H., Hulse, D.A., Kerwin, S.C. and Saunders, W.B. 2010. Minimally invasive application of a radial plate following placement of an ulnar rod in treating antebrachial fractures. Technique and case series. Vet. Comp. Orthop. Traumatol. 23, 459–467. | ||
| How to Cite this Article |
| Pubmed Style Lederer XJ, Lewis DD. Comparison of cranial vs. medial minimally invasive plate osteosynthesis applications for the stabilization of simulated radius and ulna fractures in dog cadavers. Open Vet J. 2023; 13(5): 501-509. doi:10.5455/OVJ.2023.v13.i5.1 Web Style Lederer XJ, Lewis DD. Comparison of cranial vs. medial minimally invasive plate osteosynthesis applications for the stabilization of simulated radius and ulna fractures in dog cadavers. https://www.openveterinaryjournal.com/?mno=144379 [Access: July 14, 2025]. doi:10.5455/OVJ.2023.v13.i5.1 AMA (American Medical Association) Style Lederer XJ, Lewis DD. Comparison of cranial vs. medial minimally invasive plate osteosynthesis applications for the stabilization of simulated radius and ulna fractures in dog cadavers. Open Vet J. 2023; 13(5): 501-509. doi:10.5455/OVJ.2023.v13.i5.1 Vancouver/ICMJE Style Lederer XJ, Lewis DD. Comparison of cranial vs. medial minimally invasive plate osteosynthesis applications for the stabilization of simulated radius and ulna fractures in dog cadavers. Open Vet J. (2023), [cited July 14, 2025]; 13(5): 501-509. doi:10.5455/OVJ.2023.v13.i5.1 Harvard Style Lederer, X. J. & Lewis, . D. D. (2023) Comparison of cranial vs. medial minimally invasive plate osteosynthesis applications for the stabilization of simulated radius and ulna fractures in dog cadavers. Open Vet J, 13 (5), 501-509. doi:10.5455/OVJ.2023.v13.i5.1 Turabian Style Lederer, Xiaoxiao Jade, and Daniel Dean Lewis. 2023. Comparison of cranial vs. medial minimally invasive plate osteosynthesis applications for the stabilization of simulated radius and ulna fractures in dog cadavers. Open Veterinary Journal, 13 (5), 501-509. doi:10.5455/OVJ.2023.v13.i5.1 Chicago Style Lederer, Xiaoxiao Jade, and Daniel Dean Lewis. "Comparison of cranial vs. medial minimally invasive plate osteosynthesis applications for the stabilization of simulated radius and ulna fractures in dog cadavers." Open Veterinary Journal 13 (2023), 501-509. doi:10.5455/OVJ.2023.v13.i5.1 MLA (The Modern Language Association) Style Lederer, Xiaoxiao Jade, and Daniel Dean Lewis. "Comparison of cranial vs. medial minimally invasive plate osteosynthesis applications for the stabilization of simulated radius and ulna fractures in dog cadavers." Open Veterinary Journal 13.5 (2023), 501-509. Print. doi:10.5455/OVJ.2023.v13.i5.1 APA (American Psychological Association) Style Lederer, X. J. & Lewis, . D. D. (2023) Comparison of cranial vs. medial minimally invasive plate osteosynthesis applications for the stabilization of simulated radius and ulna fractures in dog cadavers. Open Veterinary Journal, 13 (5), 501-509. doi:10.5455/OVJ.2023.v13.i5.1 |