| Research Article | ||
Open Vet. J.. 2024; 14(4): 1002-1011 Open Veterinary Journal, (2024), Vol. 14(4): 1002–1011 Original Research CT findings in seven dogs with perforating wooden skewer foreign bodies from the gastrointestinal tractAntón Costas* and Vicente CerveraAnicura Valencia Sur Veterinary Hospital, Valencia, Spain *Corresponding Author: Antón Costas. Anicura Valencia Sur Veterinary Hospital, Valencia, Spain. Email: antoncostaspereiro [at] gmail.com Submitted: 23/11/2023 Accepted: 09/03/2024 Published: 30/04/2024 © 2024 Open Veterinary Journal
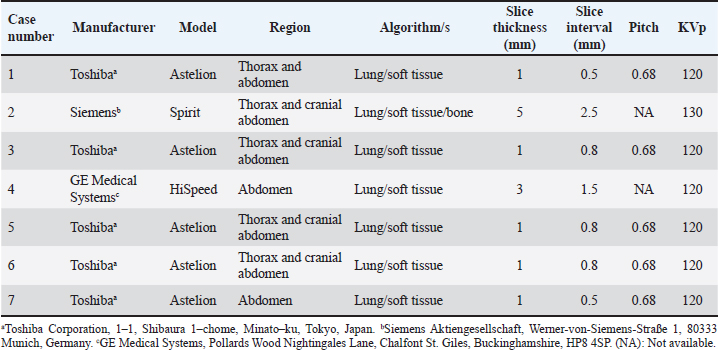
AbstractBackground: Perforating foreign bodies from the gastrointestinal tract, such as wooden skewers, are reported in the small animal literature producing inflammatory/infectious lesions in the thorax, abdomen, and musculoskeletal system, which can be life-threatening in some instances. Several imaging modalities have been used, and advanced imaging techniques have shown a great advantage in its diagnosis and pre-surgical planning. Aim: The objective of this study is to describe the computed tomographic findings in a group of seven medium to large breed dogs with perforating wooden skewers and foreign bodies migrated from the gastrointestinal tract. Methods: The medical records database was searched for dogs with a suspected diagnosis of a perforating wooden foreign body migrated from the gastrointestinal tract in which a computed tomographic study was performed. Signalment, history, and clinicopathological findings (when available) were retrieved, and the computed tomographic studies were reviewed. Results: Clinical signs vary depending on the anatomical regions affected through the perforating pathway. All foreign bodies were identified and showed a median attenuation of 79 HU, with the most common localization being the stomach followed by the jejunum. Peritoneal fat stranding surrounding the perforation site was the most frequent computed tomographic finding. The presence of peritoneal free fluid and/or gas was uncommon. Pleural effusion, pulmonary perforation, and pneumothorax were present in most of the cases with the foreign body traversing the pleural space. Pulmonary cavitary lesions were always reported when the ending tip of the wooden skewer was within the pulmonary parenchyma. Soft tissue abscessation was recognized in all cases where the ending tip was lodged in muscular or subcutaneous tissues. Conclusion: Findings supported the variability of the secondary lesions caused by this type of foreign body and the utility of computed tomography in their recognition, as well as in the identification of the wooden skewer. Keywords: Canine, Computed tomography, Gastrointestinal perforation, Ingested foreign body, Kebab stick. IntroductionDifferent types of migrating foreign bodies are described throughout the small animal literature with variable presentations and clinical signs depending on the time of presentation, route of entry, or secondary lesions along the migrating pathway. Wooden stick foreign bodies are one of the commonest in dogs, usually related to oropharyngeal lesions attributable to chewing or retrieving behavior (Griffiths et al., 2000; Nicholson et al., 2008; White and Lane, 2008), but also reported in numerous anatomical locations after distant migration from the oropharyngeal region (O’Reilly et al., 2002; Young et al., 2004; Hylands, 2007; Lamb et al., 2017), suspected or witnessed traumatic impalements (Moon et al., 2012; Perry et al., 2012; Appleby et al., 2015; Lamb et al., 2017; Bosma et al., 2022) or ingestion and migration from the gastrointestinal tract (Matteucci et al., 1999; Wyatt et al., 1999; Penninck and Mitchell, 2003; Brennan et al., 2004; Hunt et al., 2004; Sereda et al., 2009; Choi and Han, 2017; Lamb et al., 2017; Stander and Kirberger, 2011; Garcia-Pertierra et al., 2022). The latter is a relatively frequent situation, especially if the foreign body has been in contact with food because of its high palatability (Choi and Han, 2017), as is the case of wooden skewers. Once ingested, wooden skewers or pointed portions of other long wooden sticks have a tendency to perforate and migrate from the gastrointestinal tract given their length and sharply pointed ends (Hunt et al., 2004; Choi and Han, 2017), potentially causing inflammatory or infectious disease of the abdomen, thorax and/or musculoskeletal system, occasionally associated with subcutaneous draining tracts. Diverse imaging procedures such as plain radiography, fistulography/sinography, ultrasonography, computed tomography (CT), and magnetic resonance imaging (MRI) have been used alone or in combination to identify wooden foreign bodies and accompanying secondary lesions in the previously referenced literature. Various of these case reports and series highlight the utility of CT with such penetrating foreign bodies, especially as part of preoperative planning. Moreover, noncontrast CT has been evaluated and proved more accurate (sensitivity 75%, specificity 96%) than ultrasound or MRI for the detection of acute wooden foreign bodies in cadaveric dogs (Ober et al., 2008). In another study describing the CT findings in dogs with suspected wooden foreign bodies, the sensitivity and specificity of this technique were determined to be 79% and 93% (Lamb et al., 2017). The aim of this study is to describe the computed tomographic findings in a group of dogs with perforating wooden skewer foreign bodies migrated from the gastrointestinal tract. Materials and MethodsThis is a retrospective case series study design. The medical records database of the Anicura Hospital Veterinario Valencia Sur (AHVVS; Valencia, Spain), including teleradiology cases, was searched for dogs with a suspected diagnosis of a perforating wooden foreign body migrated from the gastrointestinal tract in which a computed tomographic study was performed as a part of the diagnostic investigation. The studies found were only from the teleradiology archive. Data collected from records included signalment, history, and clinicopathological findings when available. Authorized consent regarding the use of clinical data and imaging exams for publication purposes was obtained from the owners. Additional information regarding the surgical confirmation and type (when possible) of the wooden foreign body was requested from the referring colleagues. For the purposes of this study, CT images were retrieved and reviewed by a board-certified veterinary radiologist [VC, American College of Veterinary Radiology and European College of Veterinary Diagnostic Imaging (ECVDI)] and a second-year diagnostic imaging resident (AC, ECVDI second-year resident) that were not blinded to the final diagnosis. A new CT report was created for each case in consensus between both individuals. Different CT machines and protocols were used depending on the referring institution and are summarized in Table (1). All studies were performed with the patient under general anesthesia in sternal recumbency, including series before and after intravenous iodinated contrast medium administration with variable doses. DICOM images were reviewed using medical imaging viewer software (Horos Version 3.3.6, Horos Project, Annapolis, MD). Window width and level were manipulated for optimization of the region of interest (ROI) for soft tissue, lung, and bone, using multiplanar reconstructions when necessary. Maximal dimensions (long axis and thickness) of the foreign body and its attenuation value in Hounsfield Units were recorded. The HU was measured using a hand-drawn ROI including the cross-sectional area of the foreign body and avoiding gas-filled cavities. The average of three HU values was calculated. When possible, the origin and trajectory of the gastrointestinal tract were determined and described. Pulmonary and musculoskeletal lesions associated with the perforating pathway followed by the foreign body and secondary changes in the peritoneum, mediastinum, and pleural space were also described and recorded. The severity or volume of these additional findings was subjectively graded as mild, moderate, or severe. Additional objective measurements included attenuation values of the pleural effusions also by using an average of three different ROIs. Table 1. CT machines and protocols.
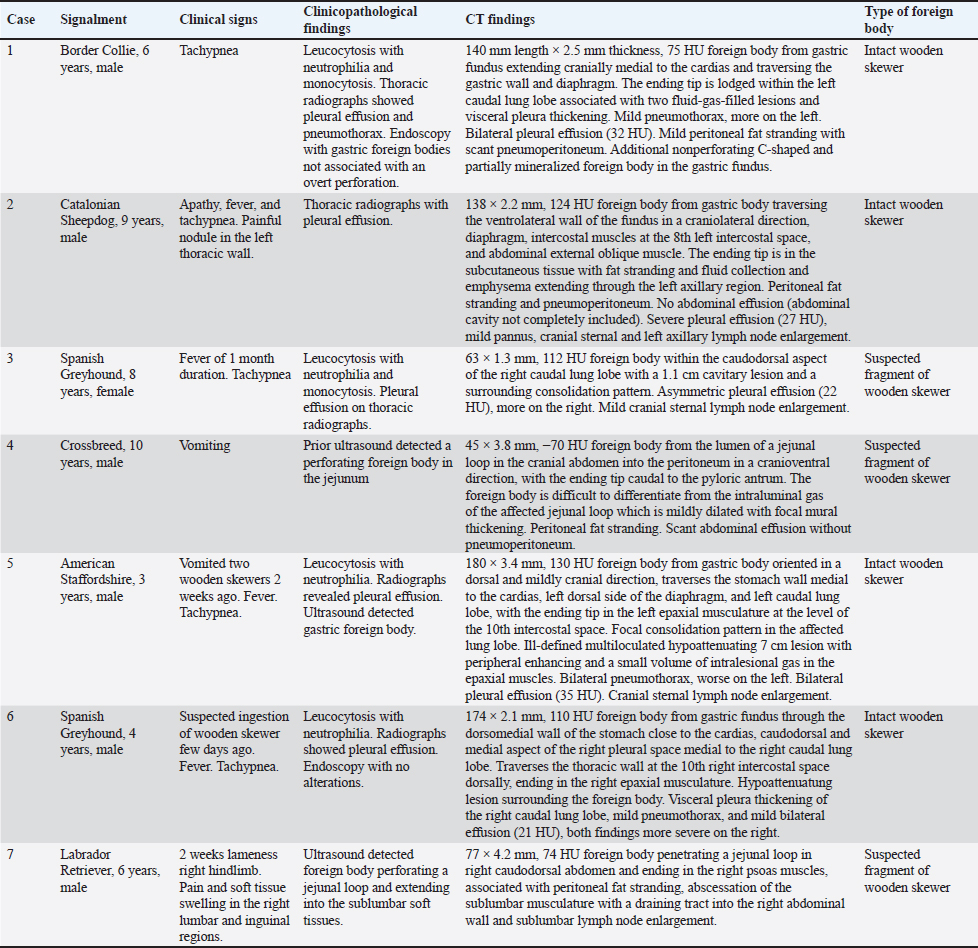
Ethical approvalNot needed for this study. ResultsA total of seven dogs were included. Signalment and clinical signs and complete CT findings of all dogs are summarized in Table (2). Before the CT examination, some patients had different imaging procedures conducted by the referral veterinarian. This information was retrieved with no review of the images by the authors of this paper and is also included in Table (2). In the cases presenting with tachypnea and pleural effusion (5/7), a foreign body was not identified radiographically and analysis of the effusion disclosed characteristics of septic exudate on cytology or culture (4/5). In the three dogs evaluated sonographically (3/7), gastric (1/3), and jejunal (2/3) perforating foreign bodies were detected, one of the latter penetrating the hypaxial musculature which showed fluid-filled lesions extending into the abdominal wall. Two dogs (2/7) had a gastroscopy performed. The foreign body was readily detected in all cases on pre-contrast images but difficult to differentiate from the surrounding soft tissues after intravenous contrast medium administration. However, they were easily identified post-contrast when surrounded by gas within the gastrointestinal tract or in the pleural space. Attenuation values for these foreign bodies ranged from −70 to 124 HU with a median attenuation value of 79 HU. The size varied from 45 to 180 mm in length and from 1.3 to 4.2 mm in thickness. The most common localization of one of the tips of the foreign body was the stomach (4/7). For all these dogs, the foreign body traversed the gastric wall and the diaphragm, entering the caudal mediastinum or caudal pleural space, and ending in the pulmonary parenchyma (1/4) or thoracic wall soft tissues (3/4). The second most common origin of the foreign body was the jejunum (2/7). In both cases, the affected jejunal loop was mildly focally dilated with mild thickening of the intestinal wall. One dog (1/7) had a foreign body within the caudodorsal aspect of the right caudal lung lobe and overt communication with the gastrointestinal tract could not be traced (Fig. 1). Secondary findings in the abdomen were detected in six dogs (Fig. 2), including: minimal to mild peritoneal fat stranding close to the perforation site with a reticular pattern (6/6), mild pneumoperitoneum (2/6), mild volume of peritoneal effusion (1/6), and right medial iliac, sacral, and inguinal lymph node enlargement (1/6). Another nonperforating c-shaped and partially mineralized foreign body was present in the gastric fundus of one patient (1/6). All dogs with thoracic involvement (5/7) had bilateral pleural effusion which was considered mild (5/5), asymmetric in one (1/5), showing attenuation values ranging from 21 to 35 HU (median 27). Four of these wooden skewers (4/5) were perforating the pulmonary parenchyma. Associated pulmonary lesions were identified and described as increased attenuation/consolidation patterns and thickening of the visceral pleura surrounding or adjacent to the foreign body (4/5), with cavitary, thin-walled, and well-defined lesions showing variable gas-fluid levels (2/5). Other findings, ranging as mild in severity, included bilateral pneumothorax (4/5), cranial sternal lymph node enlargement (3/5), pannus (2/5), and thickening of the parietal pleura (1/5). The pneumothorax was always asymmetric with more volume surrounding the site of pulmonary perforation. Variable degrees of pulmonary atelectasis were present in multiple lobes secondary to the pleural lesions, mostly in the portions surrounded by the pleural fluid or gas. Two dogs had unilateral (1/2) or bilateral (1/2) chest tubes, all associated with mild subcutaneous emphysema. For the foreign bodies with a migrating trajectory ending in the soft tissues (4/7), the most common finding in the musculoskeletal system was the presence of intramuscular and/or subcutaneous fluid- and gas-filled lesions with an irregular and markedly enhancing wall (3/4). One dog (1/4) had nonencapsulated subcutaneous fluid accumulation adjacent to the tip of the foreign body. These lesions were confirmed as abscesses in surgery. Other findings included subcutaneous fat stranding (2/4) and emphysema (2/4). No lesions were identified in the adjacent bones (0/4). All dogs underwent surgical exploration for retrieval of the foreign bodies. Four were confirmed as intact wooden skewer foreign bodies (4/7). The remaining three were wood in nature and suspected to be a fragment of a wooden skewer (3/7). DiscussionWooden skewer foreign bodies have been previously described in dogs perforating the gastrointestinal tract from the stomach or small intestines, causing inflammatory or infectious lesions in the thorax, abdomen, and/or musculoskeletal system (Penninck and Mitchell, 2003; Hunt et al., 2004; Sereda et al., 2009; Stander and Kirberger, 2011; Lamb et al., 2017; Garcia-Pertierra et al., 2022). Diagnostic imaging was proved in those studies to be helpful in identifying the foreign body itself and secondary changes, especially with the use of abdominal ultrasound, echocardiography, and advanced techniques such as CT and MRI. Table 2. Signalment, clinical signs, clinicopathological and CT findings, and type of foreign body.
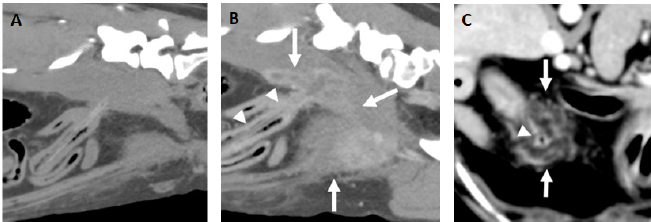
Fig. 1. Examples of fragments of wooden skewer perforating a jejunal loop. A and B. Parasagittal pre (A) and postcontrast (B) images (level 40 HU, width 250 HU) of the same patient with a fragmented wooden skewer (arrowheads) perforating the jejunum in the caudal abdomen with the ending tip penetrating the right psoas muscles. In the pre-contrast images, the portion of the foreign body embedded in the soft tissues is better visualized than in the post-contrast images, while the soft tissue abscessation is better depicted in the latter (arrows). C. Transverse post-contrast CT image (level 40 HU, width 250 HU) of another patient showing a hypoattenuating fragmented wooden skewer foreign body (arrowhead) penetrating a jejunal loop in the cranial abdomen. A marked peritoneal fat stranding is seen surrounding the small bowel loop and foreign body (arrows).
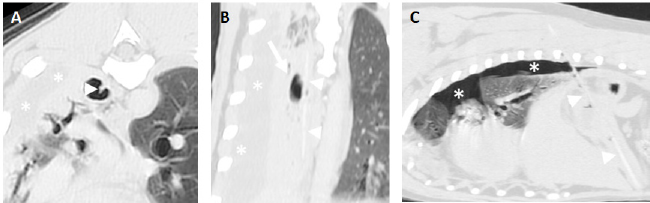
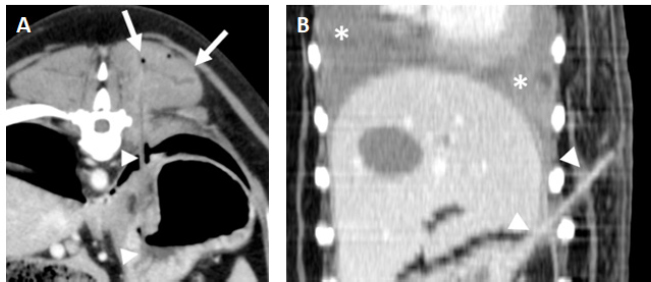
Fig. 2. A and B. Transverse and dorsal, post-contrast CT images (level −500 HU, width 1,400 HU) of the same patient showing a hyperattenuating (112 HU), 63 mm length × 1.3 mm width foreign body (arrowheads) lodged in the right caudal lung lobe and causing a small cavitary lesion (arrow). There is an asymmetric pleural effusion, more severe on the right side (asterisks). The right pulmonary lobes are decreased in volume with an almost generalized consolidation pattern, most likely secondary to atelectasis. C. Parasagittal post-contrast CT image (level −500 HU, width 1,400 HU) of a perforating wooden skewer foreign body from the stomach (arrowheads), perforating the pleural space and right caudal lung lobe which shows a focal increased attenuation and thickening of the visceral pleura. There is a mild volume of pneumothorax (asterisks). Note that the air within the pulmonary cavitary lesions or in the pleural space aids in the identification of these foreign bodies. In some of the cases presented herein, other imaging modalities were used before the CT examination. Only the ultrasound studies were able to identify the perforating foreign bodies. None of them could be detected on radiographs as they are usually radiolucent and, typically, secondary nonspecific changes are seen (Penninck and Mitchell, 2003; Hunt et al., 2004; Stander and Kirberger, 2011; Garcia-Pertierra et al., 2022). Surprisingly, in the two dogs in which a gastroscopy was performed, no perforating lesions were found despite one of them having several gastric foreign bodies identified. The experience of the operator, the presence of gastric contents, or appropriate endoscopic equipment may have played a role (Neiger and Stengel, 2021). All the wooden skewers were recognized by CT. The median attenuation was 79 HU which is slightly lower than the previously reported median attenuation of 111 HU for wooden foreign bodies (Lamb et al., 2017). This could be explained as attenuation values may vary depending on the foreign body characteristics before entering the body and absorption of fluids once ingested and migrated (Penninck and Mitchell, 2003; Lamb et al., 2017). As previously suggested (Nicholson et al., 2008; Lamb et al., 2017), the authors considered it more difficult to visualize the foreign bodies in post-contrast images as they were almost isoattenuating compared with the surrounding enhanced soft tissues. However, they were very well depicted when outlined by gas within the gastrointestinal tract or pleural space. The use of multiplanar reconstructions aided in their identification and trajectory, highlighting this tool in cases with this type of long and thin foreign objects. It has been previously speculated that the length and rigidity of this type of wooden foreign bodies prevent them from passing into the body or antrum of the stomach and cause them to perforate the wall of the fundus (Penninck and Mitchell, 2003). Accordingly, all the largest foreign bodies had one of the tips lodged in the stomach and longer perforating trajectories that extended either into the thorax or paravertebral/costal soft tissues depending on the orientation. The remaining and shorter foreign bodies were more prone to advance into distal portions of the gastrointestinal tract causing perforating lesions in the jejunum (Fig. 1). However, one of these smaller wooden foreign bodies was within a right caudal lung lobe and a clear communication with the abdomen was not seen on CT images. An origin from the digestive system, either the oesophagus or the stomach, was suspected as there was no previous history or secondary lesions supporting a theoretical inhalation or penetrating trajectory from the thoracic wall. Interestingly, this patient had a previous history of resolved abdominal effusion which could potentially be explained if a migrating pathway from the gastrointestinal tract was followed by the fragmented wooden skewer. The most common secondary finding was fat stranding with a reticular pattern adjacent to the perforation site. This is described as an abnormally increased attenuation in fat due to edema and engorgement of lymphatics (Thornton et al., 2011), found to be helpful for the localization of the underlying cause in dogs and cats (Jang et al., 2022). Despite in our cases, it was considered minimal in most of them, the presence of fat stranding adjacent to the stomach or a small bowel loop may aid in the identification of this type of perforating foreign body. In a previous study of gastrointestinal perforation in dogs and cats evaluated by radiography and ultrasonography the second most common finding was peritoneal effusion while free gas in the abdominal cavity was detected in 47% of the cases (Boysen et al., 2003). Unexpectedly, only two of our dogs showed pneumoperitoneum and one peritoneal effusion, both findings were considered mild. The presence of free gas in the peritoneum depends on several factors (Ranschaert and Rigauts, 1993; Boysen et al., 2003). We hypothesize that the small number of cases with pneumoperitoneum and abdominal effusion is related to the minor size of the perforation which may be sealed by the surrounding omentum and inflammatory changes. The chronicity in some of these patients may have also played a role. A bias may have been introduced as the entire abdominal cavity was not included in all patients. Pleural effusion was the most common finding in dogs with involvement of the thoracic cavity. The median attenuation of these fluids (27 HU) was compatible with exudate, modified transudate, or hemorrhage (Woods et al., 2018) and, in agreement with the cytologic or positive culture, finally classified as septic exudate. Pannus, defined as sheet- or mass-like tissue that replaces fibrin peel in dogs with inflammatory or reactive pleural effusion (Vansteenkiste et al., 2014), and thickening of the parietal pleural were identified less frequently and considered nonspecific features in association with the pleural effusion (Watton et al., 2017). When part of the wooden skewer was traversing the pulmonary parenchyma (Fig. 2), the surrounding lung had increased attenuation and the visceral pleura was thickened, features previously described in the perforation site secondary to grass-awn migration and most likely indicative of pneumonia and pleuritis (Baudin Tréhiou et al., 2020). Additional cavitary lesions showing gas-fluid levels with a thin and well-defined wall were present in two dogs. These were interpreted as pulmonary traumatic pseudocysts formed by the retraction of surrounding lung tissue following pulmonary laceration (Cho et al., 2015; Bertolini et al., 2020). Abscess formation could not be ruled out but was considered less likely as usually shows thicker and irregular walls (Lamb and Neiger, 2000). Secondary bilateral and asymmetric pneumothorax was present in all pulmonary perforations, and this asymmetry correlated with the side of the perforation in all cases. Another recurrent finding was seen when the ending tip of the wooden skewer was located within the paraspinal or costal soft tissues and consisted of intramuscular and subcutaneous fluid- and gas-filled lesions with an irregular and markedly enhancing wall, confirmed as abscesses (Fig. 3). In spite of being a frequent feature with penetrating foreign bodies that migrate from the lungs (Jacques et al., 2019; Griffeuille et al., 2021; Hennessey et al., 2022), this type of lesions in the paraspinal muscles are uncommon with penetrating wooden skewers from the gastrointestinal tract based in the previously published literature. Additional subcutaneous fat stranding and emphysema were also frequent; however, no bony lesions were detected. Lymph node enlargement was frequently present in the draining areas affected by the inflammatory process (Bezuidenhout, 2013) which was considered a nonspecific finding, most likely related to the local inflammatory disease.
Fig. 3. Examples of gastric foreign bodies from the stomach with the ending tip in the paravertebral or thoracic wall soft tissues. A. Transverse post-contrast CT image (level 40 HU, width 250 HU) of a dog with a wooden skewer (arrowheads) extending from the stomach and ending in the left epaxial muscles. Mild fluid accumulation and emphysema are seen surrounding the ending tip of the foreign body (arrows). B. Dorsal post-contrast CT image (level 40 HU, width 250 HU) of a dog with a wooden skewer (arrowheads) perforating the gastric wall with an oblique orientation ending in the subcutaneous tissue of the left thoracic wall. A moderate bilateral pleural effusion is seen associated with this foreign body (asterisks). The limitations of this study include those inherent to its retrospective nature. The small number of cases precluded statistical analysis. Also, the fact that all cases were retrieved from the teleradiology archive may have introduced historical data recording inaccuracies, as well as variability from the multiple attending surgeons and referral institutions. ConclusionIn conclusion, in dogs with ingested wooden skewers that perforate and migrate from the gastrointestinal tract, CT can effectively identify them, especially in pre-contrast images, and the diverse secondary lesions, most of the times with concurrent affection of several body parts. Pneumoperitoneum or peritoneal effusion were uncommon findings contrary to what is expected with gastrointestinal perforation. Paraspinal abscesses and pulmonary lesions were relatively common in the presence of a large gastric wooden skewer. The authors recommend this technique for the diagnosis and surgical planning of this particular type of wooden foreign body. Conflict of interestThe authors declare that there is no conflict of interest. FundingThis research received no specific grant. Authors’ contributionsAll authors contributed to the conception and design of the article. AC conducted the retrieval of the data and literature review. VC revised the final manuscript. All authors read and approved the article. Data availabilityAll data supporting the findings of this study are available within the manuscript. ReferencesAppleby, R., Zur Linden, A., Singh, A., Finck, C. and Crawford, E. 2015. Computed tomography diagnosis of a thoracic and abdominal penetrating foreign body in a dog. Can. Vet. J. 56, 1149–1152. Baudin Tréhiou, C., Gibert, S., Sériot, P., Dunié-Mérigot, A. and Blond, L. 2020. CT is helpful for the detection and presurgical planning of lung perforation in dogs with spontaneous pneumothorax induced by grass awn migration: 22 cases. Vet. Radiol. Ultrasound. 61, 157–166. Bertolini, G., Briola, C., Angeloni, L., Costa, A., Rocchi, P. and Caldin, M. 2020. Trauma-associated pulmonary laceration in dogs-a cross sectional study of 364 dogs. Vet. Sci. 7, 41. Bezuidenhout, A.J. 2013. The lymphatic system. In Miller’s anatomy of the dog, 4th edition. Eds., Evans, H. and de Lahunta, A. St Louis, MO: Elseivier Saunders, pp: 535–562. Bosma, F., Gerritsen, R., Visser, J. and Passon-Vastenburg, M. 2022. Contrast-enhanced CT findings in a dog with a wood foreign body in the vertebral canal. Vet. Radiol. Ultrasound. 63, 6–10. Boysen, S.R., Tidwell, A.S. and Penninck, D.G. 2003. Ultrasonographic findings in dogs and cats with gastrointestinal perforation. Vet. Radiol. Ultrasound. 44, 556–564. Brennan, S.F., Connery, N., Tobin, E., Mooney, C.T. and Jones, B.R. 2004. Gastrocutaneous fistula as a result of migration of a foreign body in a dog. J. Small Anim. Pract. 45, 304–306. Cho, H.J., Jeon, Y.B., Ma, D.S., Lee, J.N. and Chung, M. 2015. Traumatic pulmonary pseudocysts after blunt chest trauma: prevalence, mechanisms of injury, and computed tomography findings. J. Trauma Acute Care Surg. 79, 425–430. Choi, Y.D. and Han, H.J. 2017. Pyothorax induced by an intrathoracic foreign body in a miniature dachshund: migration of a popsicle stick from the stomach. J. Vet. Med. Sci. 79, 1398–1403. Garcia-Pertierra, S., Das, S., Burton, C., Barnes, D., Murgia, D., Anderson, D., Kulendra, N., Harris, K. and Forster, K. 2022. Surgical management of intrathoracic wooden skewers migrating from the stomach and duodenum in dogs: 11 cases (2014-2020). J. Small Anim. Pract. 63, 403–411. Griffeuille, E., Seriot, P., Baudin-Tréhiou, C., Gibert, S., Blond, L., Poujol, L. and Dunié-Mérigot, A. 2021. Comparison of computed tomography and surgical findings and investigation of their associations with outcomes for dogs with sublumbar abscesses. J. Am. Vet. Med. Assoc. 259, 1300–1308. Griffiths, L.G., Tiruneh, R., Sullivan, M. and Reid, S.W. 2000. Oropharyngeal penetrating injuries in 50 dogs: a retrospective study. Vet. Surg. 29, 383–388. Hennessey, E., Cassel, N., Nuth, E. and Biller, D. 2022. CT can identify characteristic features of hypaxial muscle abscesses in dogs due to presumed migrating vegetal foreign material as well as additional changes along the migratory tract in other anatomic regions. Vet. Radiol. Ultrasound. 63, 691–698. Hunt, G.B., Worth, A. and Marchevsky, A. 2004. Migration of wooden skewer foreign bodies from the gastrointestinal tract in eight dogs. J. Small Anim. Pract. 45, 362–367. Hylands, R. 2007. Veterinary diagnostic imaging: 9-cm wooden foreign body lodged in the sternocephalic muscle in the caudal part of the neck. Can. Vet. J. 48, 643–645. Jacques, D., Meige, F. and Thierry, F. 2019. Clinical, computed tomographic, surgical findings and outcome in dogs with sublumbar abscessation: 16 cases (2013-2019). J. Small Anim. Pract. 63, 147–153. Jang, S., Lee, S. and Choi, J. 2022. CT imaging features of fat stranding in cats and dogs with abdominal disorder. J. Vet. Sci. 23(6), e70. Lamb, C.R. and Neiger, R. 2000. Radiology corner: differential diagnosis of pulmonary cavitary lesions. Vet. Radiol. Ultrasound. 4, 340–341. Lamb, C.R., Pope, E.H. and Lee, K.C. 2017. Results of computed tomography in dogs with suspected wooden foreign bodies. Vet. Radiol. Ultrasound. 58, 144–150. Matteucci, M.L., Spaulding, K., Dassler, C. and Lee, D. 1999. Ultrasound diagnosis: intra-abdominal wood foreign body. Vet. Radiol. Ultrasound. 40, 513–516. Moon, S.J., Lee, J.H., Jeong, S.W., Kim, J.W. and Park, H.M. 2012. Chronic bronchocutaneous fistula caused by toothpick foreign body in a Maltese dog. J. Vet. Med. Sci. 74, 651–655. Neiger, R. and Stengel, C. 2021. Gastrointestinal endoscopy. In Veterinary endoscopy for the small animal practitioner. Ed., McCarthy, T.C. Hoboken, NJ: Wiley-Blackwell. Nicholson, I., Halfacree, Z., Whatmough, C., Mantis, P. and Baines, S. 2008. Computed tomography as an aid to management of chronic oropharyngeal stick injury in the dog. J. Small Anim. Pract. 49, 451–457. Ober, C.P., Jones, J.C., Larson, M.M., Lanz, O.I. and Werre, S.R. 2008. Comparison of ultrasound, computed tomography, and magnetic resonance imaging in detection of acute wooden foreign bodies in the canine manus. Vet. Radiol. Ultrasound. 49, 411–418. O’Reilly, A., Beck, C., Mouatt, J.G. and Stenner, V.J. 2002. Exophthalmos due to a wooden foreign body in a dog. Aust. Vet. J. 80, 268–271. Penninck, D. and Mitchell, S.L. 2003. Ultrasonographic detection of ingested and perforating wooden foreign bodies in four dogs. J. Am. Vet. Med. Assoc. 223, 206–209. Perry, B., Witsberger, T., Young, B. and Howe, L. 2012. What is your diagnosis? Chronic wooden foreign body. J. Am. Vet. Med. Assoc. 241, 429–431. Ranschaert, E. and Rigauts, H. 1993. Confined gastric perforation: ultrasound and computed tomographic diagnosis. Abdom. Imaging. 18, 318–319. Sereda, N.C., Towl, S., Maisenbacher, H.W. 3rd, Bleweis, M.S., Levy, J.K., Byrne, B.J., Ellison, G.W., Shih, A., Coomer, A.R. and Estrada, A.H. 2009. Intracardiac foreign body in a dog. J. Vet. Cardiol. 11, 53–58. Stander, N. and Kirberger, R.M. 2011. Diagnostic imaging of migrating kebab (sosatie) sticks--a review of 8 cases. J. S. Afr. Vet. Assoc. 82, 160–165. Thornton, E., Mendiratta-Lala, M., Siewert, B. and Eisenberg, R.L. 2011. Patterns of fat stranding. AJR Am. J. Roentgenol. 197, 1–14. Vansteenkiste, D.P., Lee, K.C. and Lamb, C.R. 2014. Computed tomographic findings in 44 dogs and 10 cats with grass seed foreign bodies. J. Small Anim. Pract. 55, 579–584. Watton, T.C., Lara-Garcia, A. and Lamb, C.R. 2017. Can malignant and inflammatory pleural effusions in dogs be distinguished using computed tomography? Vet. Radiol. Ultrasound. 58, 535–541. White, R. and Lane, J. 2008. Pharyngeal stick penetration injuries in the dog. J. Small Anim. Pract. 29, 13–35. Woods, S.J., Spriet, M., Safra, N., Cissell, D.D. and Borjesson, D.L. 2018. Hounsfield units are a useful predictor of pleural effusion cytological type in dogs but not in cats. Vet. Radiol. Ultrasound. 59, 405–411. Wyatt, K.M., Marchevsky, A.M. and Kelly, A. 1999. An enterovesical foreign body in a dog. Aust. Vet. J. 77, 27–29. Young, B., Klopp, L., Albrecht, M. and Kraft, S. 2004. Imaging diagnosis: magnetic resonance imaging of a cervical wooden foreign body in a dog. Vet. Radiol. Ultrasound. 45, 538–541. | ||
| How to Cite this Article |
| Pubmed Style Costas A, Cervera V. CT findings in seven dogs with perforating wooden skewer foreign bodies from the gastrointestinal tract. Open Vet. J.. 2024; 14(4): 1002-1011. doi:10.5455/OVJ.2024.v14.i4.7 Web Style Costas A, Cervera V. CT findings in seven dogs with perforating wooden skewer foreign bodies from the gastrointestinal tract. https://www.openveterinaryjournal.com/?mno=178616 [Access: January 25, 2026]. doi:10.5455/OVJ.2024.v14.i4.7 AMA (American Medical Association) Style Costas A, Cervera V. CT findings in seven dogs with perforating wooden skewer foreign bodies from the gastrointestinal tract. Open Vet. J.. 2024; 14(4): 1002-1011. doi:10.5455/OVJ.2024.v14.i4.7 Vancouver/ICMJE Style Costas A, Cervera V. CT findings in seven dogs with perforating wooden skewer foreign bodies from the gastrointestinal tract. Open Vet. J.. (2024), [cited January 25, 2026]; 14(4): 1002-1011. doi:10.5455/OVJ.2024.v14.i4.7 Harvard Style Costas, A. & Cervera, . V. (2024) CT findings in seven dogs with perforating wooden skewer foreign bodies from the gastrointestinal tract. Open Vet. J., 14 (4), 1002-1011. doi:10.5455/OVJ.2024.v14.i4.7 Turabian Style Costas, Antón, and Vicente Cervera. 2024. CT findings in seven dogs with perforating wooden skewer foreign bodies from the gastrointestinal tract. Open Veterinary Journal, 14 (4), 1002-1011. doi:10.5455/OVJ.2024.v14.i4.7 Chicago Style Costas, Antón, and Vicente Cervera. "CT findings in seven dogs with perforating wooden skewer foreign bodies from the gastrointestinal tract." Open Veterinary Journal 14 (2024), 1002-1011. doi:10.5455/OVJ.2024.v14.i4.7 MLA (The Modern Language Association) Style Costas, Antón, and Vicente Cervera. "CT findings in seven dogs with perforating wooden skewer foreign bodies from the gastrointestinal tract." Open Veterinary Journal 14.4 (2024), 1002-1011. Print. doi:10.5455/OVJ.2024.v14.i4.7 APA (American Psychological Association) Style Costas, A. & Cervera, . V. (2024) CT findings in seven dogs with perforating wooden skewer foreign bodies from the gastrointestinal tract. Open Veterinary Journal, 14 (4), 1002-1011. doi:10.5455/OVJ.2024.v14.i4.7 |