| Case Report | ||
Open Vet. J.. 2023; 13(12): 1752-1759 Open Veterinary Journal, (2023), Vol. 13(12): 1752-1759 Case Report Navicular bone fracture and severe deep digital flexor tendinopathy after palmar digital neurectomy in two horsesElizabeth A. Larsen1, Megan R. Williams2*, Mike J. Schoonover2, Kelsey A. Jurek3, Jenna M. Young4 and Hugh R. Duddy51Large Animal Clinical Sciences Department, University of Tennessee College of Veterinary Medicine, Knoxville, TN 37996, USA 2Veterinary Clinical Sciences Department, College of Veterinary Medicine, Oklahoma State University, Stillwater, OK 74078, USA 3Department of Clinical Sciences, Carlson College of Veterinary Medicine, Oregon State University, Corvallis, Oregon 97331, USA 4Veterinary Population Medicine Department, College of Veterinary Medicine, University of Minnesota, Saint Paul, MN 55108, USA 5Department of Veterinary Clinical Sciences, College of Veterinary Medicine, Purdue University, West Lafayette, IN 47907, USA *Corresponding Author: Megan R. Williams. Veterinary Clinical Sciences Department, College of Veterinary Medicine, Oklahoma State University, Stillwater, OK. Email: megan.willams12 [at] okstate.edu Submitted: 06/09/2023 Accepted: 07/12/2023 Published: 31/12/2023 © 2023 Open Veterinary Journal
AbstractBackground: Navicular syndrome is a common cause of forelimb lameness in horses. Beyond changes to the navicular bone itself, horses with a clinical diagnosis of navicular syndrome often have pathology associated with other components of the navicular apparatus, including the navicular bursa, deep digital flexor (DDF) tendon, collateral sesamoidean ligaments, and impar ligament. Palmar digital neurectomy (PDN) is often used as a salvage procedure for horses diagnosed with navicular syndrome that become unresponsive to medical management. There are many potential complications associated with PDN, some of which are debilitating. Case Description: This report describes two cases of navicular bone fracture with severe DDF tendinopathy and distal interphalangeal joint subluxation/hyperextension that occurred 12 and 19 weeks after bilateral forelimb PDN. Conclusion: These two cases highlight the importance of proper patient selection before PDN due to the high incidence of undiagnosed soft tissue pathology in conjunction with radiographic evidence of navicular syndrome. Advanced imaging of the digit is recommended to identify and characterize any soft tissue pathology associated with the navicular apparatus before pursuing PDN to avoid disease progression and catastrophic injury. Keywords: Horse, Navicular syndrome, Navicular bone fracture, Palmar digital neurectomy, Deep digital flexor tendon. IntroductionNavicular syndrome is a chronic, progressive condition affecting the navicular bone and its associated soft tissue structures and is a frequent cause of lameness in performance horses (Blunden et al., 2006; Waguespack and Hanson, 2010; Dyson et al., 2011; Waguespack and Hanson, 2011). Due to the close association of the collateral sesamoidean ligaments, deep digital flexor (DDF) tendon, navicular bursa, and impar ligament, there are often concurrent injuries in addition to navicular bone degenerative changes contributing to a clinical presentation of lameness (Dyson et al., 2003; Matthews et al., 2003; Busoni et al., 2005; Dyson et al., 2005; Blunden et al., 2006; Dyson and Murray, 2007; Sampson et al., 2009; Dyson et al., 2011; Dyson, 2015). Treatment options for navicular syndrome include therapeutic shoeing, systemic anti-inflammatories, intra-synovial injection of various medications and orthobiologics, systemic bisphosphonates, osteostixis of the navicular bone (Brock et al., 2023), and palmar digital neurectomy (PDN) (Matthews et al., 2003; Piccot-Crézollet et al., 2005; Schoonover et al., 2005; Maher et al., 2008; Bell et al., 2009; Dyson et al., 2011; Waguespack and Hanson, 2011; Dyson, 2015; Daniel et al., 2016). Although PDN does provide pain relief to horses suffering from lameness associated with navicular disease, it does not treat the existing pathology and can be associated with catastrophic complications such as navicular bone fracture and DDF tendon rupture (Kaser-Hotz et al., 1991a; Jackman et al., 1993; Matthews et al., 2003; Maher et al., 2008; Waguespack and Hanson, 2010; Dyson et al., 2011; Waguespack and Hanson, 2011; Dyson, 2015). While complications of PDN are well known, there are few published descriptions of catastrophic injury following PDN (Rose, 1977; Colles, 2001). The objective of this report is to describe two cases of concurrent navicular bone fracture, severe DDF tendinopathy, and distal interphalangeal joint (DIPJ) subluxation occurring after bilateral forelimb PDN. Case DetailsHorse 1 was a 12-year-old Quarter Horse gelding previously diagnosed with severe bilateral forelimb navicular syndrome of unknown duration donated to Oklahoma State University for inclusion in the College of Veterinary Medicine’s teaching herd. At the time of donation, the gelding displayed a bilateral grade 3/5 forelimb lameness [AAEP 0-5 Scale (American Association of Equine Practitioners, 1991)] but was deemed comfortable enough for pasture turnout with medical management. Over the next 2 years, the horse was housed in pasture turnout with several other teaching horses. Serial lameness evaluations were performed for teaching purposes or when the horse’s lameness was observed to worsen. At each evaluation, the lameness was eliminated with diagnostic anesthesia of the palmar digital nerves. The lameness was managed with intermittent systemic nonsteroidal anti-inflammatories as well as intermittent injection of the DIPJ or navicular bursa with corticosteroids and hyaluronic acid. Progression of navicular bone degeneration was well documented over time with plain radiography.
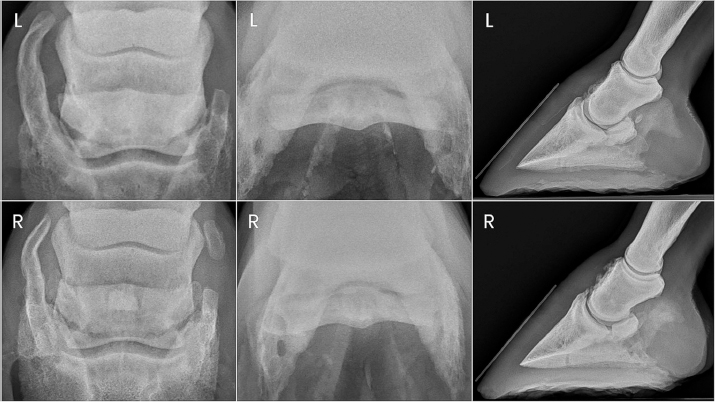
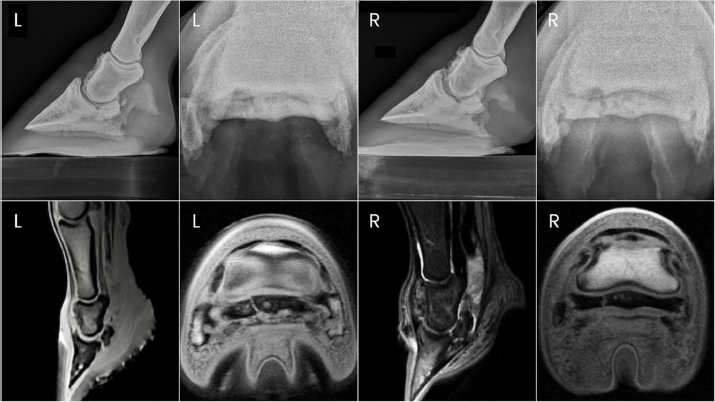
Fig. 1. Preoperative radiographs of the digits of horse 1. Two years after donation, the gelding had progressed to displaying a grade 4/5 left forelimb lameness. This lameness was eliminated with diagnostic anesthesia of the left palmar digital nerves at the level of the proximal interphalangeal joint and replaced by a grade 4/5 right forelimb lameness. The right forelimb lameness was then eliminated with diagnostic anesthesia of the right palmar digital nerves in a similar fashion. PDN was performed as a salvage procedure to maintain pasture soundness. Abnormalities noted on the immediate preoperative radiographs included severe navicular bone degeneration bilaterally, osteoarthritis of the proximal and DIPJs bilaterally, and a focal area of mineralization in the area of the left DDF tendon just proximal to the navicular bone (Fig. 1). Horse 2 was a 14-year-old Quarter Horse gelding previously diagnosed with moderate bilateral forelimb navicular syndrome of 3 years duration and donated to Oklahoma State University for inclusion in the College of Veterinary Medicine’s teaching herd. At the time of donation, the gelding displayed a bilateral grade 3/5 forelimb lameness but was deemed comfortable enough for pasture turnout with medical management. Over the next 2 years, the horse was housed in pasture turnout with several other teaching horses. Serial lameness evaluations were performed for teaching purposes or when the horse’s lameness was observed to worsen. At each evaluation, the lameness was eliminated with diagnostic anesthesia of the palmar digital nerves. The lameness was managed with intermittent systemic nonsteroidal anti-inflammatories and intermittent injection of the DIPJ with corticosteroids and hyaluronic acid. Progression of navicular bone degeneration was well documented over time with plain radiography. Two years after donation, the gelding progressed to displaying a grade 4/5 right forelimb lameness. This lameness was eliminated with diagnostic anesthesia of the right palmar digital nerves at the level of the proximal interphalangeal joint and replaced by a grade 3/5 left forelimb lameness. The left forelimb lameness was then eliminated with diagnostic anesthesia of the left palmar digital nerves in a similar fashion. PDN was performed as a salvage procedure to maintain pasture soundness. Preoperative radiographs showed severe bilateral navicular bone degeneration with focal mineralization of the DDF tendon bilaterally (Fig. 2). Both horses were anesthetized and maintained on a total intravenous anesthesia protocol. After induction, each horse was placed in dorsal recumbency and both forelimbs were extended using a hoist. The distal forelimbs were aseptically prepared and draped in a routine fashion. Bilateral forelimb PDN was performed using the guillotine technique in horse 1 (Matthews et al., 2003) and the pull-through technique in horse 2 (Maher et al., 2008). Sterile bandages consisting of nonadherent dressings covered by cotton combine rolls secured with brown roll gauze and cohesive tape were placed, and the horses recovered from anesthesia unassisted without complications. Postoperatively, both horses were administered a tapering dose of phenylbutazone administered orally at 2.2 mg/kg twice daily for 2 days followed by 2.2 mg/kg once daily for 5 days. Horses remained on stall rest for 2 weeks, followed by limited small paddock turnout for 6 (horse 1) or 5 (horse 2) weeks with controlled hand walking before resuming unrestricted pasture turnout. Distal limb bandages were maintained until suture removal 2 weeks postoperatively and replaced with standing wraps for an additional 2 or 4 weeks, respectively. Horse 1 remained pasture sound until day 84 post-PDN when he was presented for an abnormal gait with both toes displaying a mild dorsal elevation off the ground when weight bearing. Radiographs of the digits revealed parasagittal fractures of both forelimb navicular bones with hyperextension of both DIPJs (Fig. 3). Severe fiber pattern disruption of the DDF tendon was noted on ultrasound of both forelimb palmar pastern regions suggestive of severe DDF tendinopathy or rupture. Humane euthanasia was elected due to the severity of the pathology and poor prognosis. Postmortem magnetic resonance imaging (MRI) was performed on the forelimbs, which identified marked navicular bone degeneration with obliquely oriented, complete fractures of the lateral quarter of the navicular bone bilaterally, complete rupture of the DDF tendon extending from the distal aspect of the first phalanx to the navicular bone in the right forelimb, and nearly complete rupture of the DDF tendon in the left forelimb (Fig. 3). Additional findings of note in both forelimbs were hyperextension of the DIPJ, significant navicular bursitis with probable bursal adhesions, and desmitis of the impar, collateral sesamoidean, and distal digital annular ligaments.
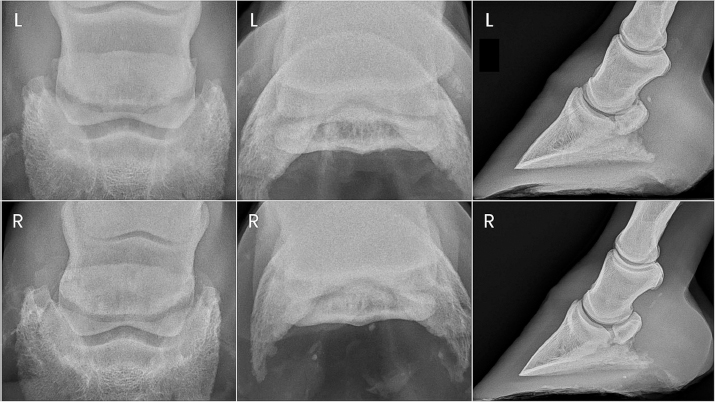
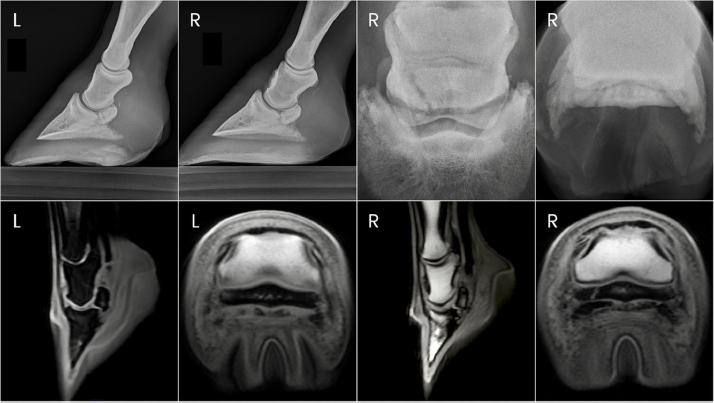
Fig. 2. Preoperative radiographs of the digits of horse 2. Horse 2 remained comfortable postoperatively with no appreciable lameness until approximately day 129, at which time a mild and inconsistent grade 4/5 RF lameness was noted. On day 136 post-PDN, the gelding was presented for student teaching of radiographic techniques. Radiographs were taken of both front digits, which revealed a parasagittal fracture of the right forelimb navicular bone and mild hyperextension of the right DIPJ (Fig. 4). Ultrasound revealed severe fiber pattern disruption of the DDF tendon suggestive of severe tendinopathy or rupture in the distal pastern region of both the right and left forelimbs. Humane euthanasia was elected due to the severity of the pathology and poor prognosis. Postmortem MRI was performed on both forelimbs revealing marked bilateral navicular bone degeneration with an obliquely oriented complete fracture of the lateral quarter of the navicular bone on the right forelimb, and bilateral severe DDF tendinopathy with almost complete rupture of the DDF tendon at the level of the navicular bone (Fig. 4). Additional findings of note in both forelimbs were significant navicular bursitis with probable bursal adhesions, enthesopathy of the flexor surface of the third phalanx at the DDF tendon insertion site, and impar, collateral sesamoidean ligament, and distal digital annular ligament desmopathy. DiscussionBoth cases described here report the occurrence of navicular bone fracture, DDF tendinopathy, and DIPJ subluxation after PDN in horses restricted to pasture turnout with no forced exercise. While these complications of PDN are well known, to the best of authors’ knowledge, they have not been reported specifically in horses not in work. PDN is typically performed to achieve soundness for some degree of athletic activity, creating a significant risk for catastrophic injury following surgery in a horse with structural unsoundness related to severe navicular bone degeneration and/or soft tissue injury. A search of the current literature identified only one case report of DDF tendon rupture and bilateral subluxation of the DIPJs after PDN; at the time of DDF tendon rupture, the horse was 8 weeks post PDN and it was not specified whether or not the horse had yet returned to work (Rose, 1977). The fact that both horses discussed here sustained such substantial complications of PDN while not in any kind of forced exercise program suggests that even the mechanical forces experienced from normal daily activity may predispose horses with significant pathology to catastrophic injury following PDN. This calls into question the rationale for performing PDN as a salvage procedure for horses with severe pathology. Candidates for PDN should be evaluated thoroughly to ensure appropriate case selection. In addition to navicular bone pathology, horses with navicular syndrome often have identifiable lesions of the DDF tendon and other soft tissue structures of the navicular apparatus. Specifically, there is a positive correlation between navicular bone abnormalities and concurrent DDF tendinopathy (Dyson et al., 2003, 2005; Blunden et al., 2006; Dyson and Murray, 2007; Dyson et al., 2011; Dyson, 2015). Severe, persistent lameness that improves following palmar digital anesthesia in the absence of radiographic evidence of navicular bone degeneration can be suggestive of soft tissue injury within the navicular apparatus including but not limited to the DDF tendon. MRI remains the gold standard for identifying musculoskeletal pathology of the distal limb (Dyson et al., 2003, 2005; Zubrod and Barrett, 2007; Blunden et al., 2009; Maher et al., 2011; Acutt et al., 2022). Unfortunately, the availability of MRI is sometimes limited, or MRI may not be financially feasible for some clients. Although technically challenging, the DDF tendon can be imaged with ultrasound as far distally as the proximal border of the navicular bone (Acutt et al., 2022); however, only 10%–28% of DDF tendinopathy lesions diagnosed with MRI were identified by ultrasound (Whitcomb, 2005, 2008; Acutt et al., 2022). Horses with core or linear lesions of the DDF tendon have been suggested to be poor candidates for PDN, as they have been shown to experience residual or early recurrent lameness postoperatively (Gutierrez-Nibeyro et al., 2015). DDF tendinopathy was a concern in both of the horses in the current report specifically due to the mineral opacities in the area of the DDF tendon noted on preoperative radiographs. Advanced imaging, such as MRI, was not obtained in either of these cases preoperatively due to a lack of availability and recognition that the PDN procedure was being performed to salvage the horses for pasture soundness only.
Fig. 3. Antemortem radiographs and postmortem MRI images of horse one showing bilateral navicular bone fractures, DIPJ hyperextension, and DDF tendon compromise.
Fig. 4. Ante-mortem radiographs and postmortem MRI images of horse two showing the right forelimb navicular bone fracture and bilateral DDF tendon compromise. Injecting the navicular bursa with corticosteroids is a common treatment for navicular syndrome, often before PDN. Navicular bursa injections with corticosteroids were performed in horse 1 and did provide short-term improvement. Multiple techniques for approaching the navicular bursa have been described, including a tendon-sparing technique (Schramme et al., 2000; Piccot-Crézollet et al., 2005; Daniel et al., 2016). The tendon-sparing technique, however, requires more technical expertise and carries a relatively high risk of synovial penetration when the DIPJ and/or digital flexor tendon sheath are distended. As a result, more traditional approaches where the needle is passed through the DDF tendon are often used. Passing the needle through the DDF tendon certainly induces iatrogenic damage, and DDF tendinopathy following centesis of the navicular bursa has been reported (Froydenlund et al., 2017). In addition, high local corticosteroid concentrations can delay tendon healing (Hoegaerts et al., 2005; Froydenlund et al., 2017). DDF tendon rupture with navicular bone fracture has been reported in one horse receiving multiple (four) navicular bursa corticosteroid injections over a 4-month period (Hoegaerts et al., 2005). While it is possible that prior navicular bursa injections with corticosteroids played a role in the ultimate catastrophic injury of horse 1, horse 2 had no known history of navicular bursa injections before PDN. Both horses in the current report sustained navicular bone fractures following PDN. In general, navicular bone fractures are uncommon and usually occur as the result of a traumatic insult (Németh and Dik, 1985; Kaser-Hotz et al., 1991b; Baxter et al., 1995; Colles, 2001, 2011). While it has been suggested that severe degenerative pathology and associated demineralization of the navicular bone can lead to fracture, a case series of 40 horses presenting for navicular bone fractures did not describe any cases with existing navicular bone pathology, and only 1 case had previously undergone PDN (Németh and Goedegebuure, 1982; Baxter et al., 1995; Colles, 2001, 2011). It has been hypothesized that sudden unexpected movements may cause the horse to overcome the proprioceptive protective factors of the navicular bone and cause the middle phalanx to put increased mechanical forces on the navicular bone. This results in excess strain on the collateral sesamoidean ligaments of the navicular bone, and the resultant tensile forces at its attachments would cause the navicular bone to fracture in a sagittal/parasagittal plane as seen in the two cases described here (Colles, 2001, 2011). Kinematics of the foot has been shown to be altered in horses after anesthesia of the navicular apparatus at both the walk and the trot (Buchner et al., 1996; Weishaupt et al., 2006; Lawson et al., 2007; Moorman et al., 2013; Serra Bragança et al., 2021). More specifically, lameness localized to the heel caused an increase in break-over duration and maximum cranial acceleration at the walk and trot, which then returned to baseline after anesthesia of the palmar digital nerves at the level of the proximal interphalangeal joint (Moorman et al., 2013, 2014). It is reasonable to conclude that the protective alteration in movement and forces applied to the navicular apparatus in the horses of this report reverted to normal or near-normal after PDN, which likely allowed for accelerated progression of the pre-existing pathology. It is the authors’ suspicion that the desensitization of the heel following PDN led to increased loading on significantly compromised DDF tendons and that this increased loading led to severe DDF tendinopathy and destabilization of the DIPJ. The resulting excessive tension on the collateral sesamoidean ligaments combined with greater forces imposed on the navicular bone by the middle phalanx likely led to the fracture of the navicular bone. It is also possible that the significant degenerative changes of the navicular bones predisposed these two horses to fracture without an inciting traumatic event, and that DDF tendinopathy and DIPJ subluxation occurred following navicular bone fracture. The lack of severe lameness in both of these horses, despite unilateral or bilateral navicular bone fracture and severe bilateral DDF tendinopathy, indicates the overt risks of desensitization of the foot after PDN. Navicular bone fractures left to heal without internal fixation are reported to form only a fibrous union with delayed ossification, leaving radiographic evidence of a fracture for the rest of the horse’s life (Arnbjerg, 1979). The authors cannot definitively pinpoint when in the post-PDN period the navicular bone fracture occurred in horse 2, as lack of evidence of radiographic healing does not necessarily mean the fracture was acute. The degree of osseus proliferation of the dorsal aspect of the middle phalanx seen in the right forelimb of horse 2 post-PDN which was not evident on radiographs before surgery suggests chronic destabilization of the DIPJ, whether due to progression of DDF tendinopathy, delayed diagnosis of navicular bone fracture, or both. However, it is notable that horse 1 had some evidence of osseous proliferation of the dorsal aspect of the middle phalanx bilaterally before PDN. The authors speculate that this suggests a more severe pre-existing DDF tendinopathy resulting in subclinical destabilization of the DIPJs even before PDN in horse 1. A limitation in this report is the lack of advanced imaging, specifically MRI, before PDN which would have allowed identification of lesions in the soft tissue structures of the navicular apparatus. Preoperative distal limb MRI would have identified all pre-existing pathology and improved the surgeons’ ability to assess the risk of catastrophic injury after PDN. An additional limitation is the surgical technique and postoperative rehabilitation decisions were made at the discretion of the surgeon managing the case and were not standardized between the two cases. However, the differences noted were relatively minor and unlikely to result in significant differences in outcomes between cases. ConclusionThis case report emphasizes that case selection should be carefully considered before PDN due to the strong association of soft tissue injuries with radiographic changes of the navicular bone. Patients with severe radiographic evidence of navicular bone degenerative changes and/or mineralization in the DDF tendon may be poor candidates for PDN even if only for salvage purposes, and clients should be advised accordingly. Advanced imaging such as MRI is essential to diagnose significant soft tissue injuries associated with the navicular apparatus, before pursuing PDN, to evaluate whether the horse is a poor surgical candidate and thus avoid catastrophic injury. AcknowledgmentsThe authors would like to thank their colleagues at the Oklahoma State University Boren Veterinary Medical Hospital. Authors contributionThe horses described in this case were a part of the Oklahoma State University Teaching Herd. Case management for horse 1 was performed by M. Williams, J. Young, and H. Duddy. Case management for horse 2 was performed by M. Schoonover, H. Duddy, and K. Jurek. Contributions to the preparation of the manuscript were made by E. Larsen, M. Williams, and M. Schoonover. All authors edited the manuscript and gave their approval for the final version. Conflict of interestThe authors declare that they have no conflicts of interest. FundingNo financial support or donations of equipment or drugs were received for the development of this report or in the diagnosis and treatment of the animals about which this report was written. Data availabilityAdditional imaging is available upon request. ReferencesAcutt, E.V., Contino, E.K., Frisbie, D.D. and Barrett, M.F. 2022. Deep digital flexor tendon lesions in the pastern are associated with the presence of distal tendinopathy. Equine Vet. J. 54, 502–512. American Association of Equine Practitioners. 1991. Guide for veterinary service and judging of equestrian events, 4th ed. Lexington, KY: AAEP. Arnbjerg, J. 1979. Spontaneous fracture of the navicular bone in the horse. Nord. Vet. Med. 31, 429–435. Baxter, G.M., Ingle J.E. and Trotter, GW. 1995. Complete navicular bone fractures in horses. Proc. Am. Assoc. Equine. Pract. 41, 243–244. Bell, C.D., Howard, R.D., Taylor, D.S., Voss, E.D. and Werpy, N.M. 2009. Outcomes of podotrochlear (navicular) bursa injections for signs of foot pain in horses evaluated via magnetic resonance imaging: 23 cases (2005-2007). J. Am. Vet. Med. Assoc. 234, 920–925. Blunden, A., Dyson, S., Murray, R. and Schramme, M. 2006. Histopathology in horses with chronic palmar foot pain and age-matched controls. Part 2: The deep digital flexor tendon. Equine Vet. J. 38, 23–27. Blunden, A., Murray, R. and Dyson, S. 2009. Lesions of the deep digital flexor tendon in the digit: a correlative MRI and post mortem study in control and lame horses. Equine Vet. J. 41, 25–33. Brock, B.A., Greer, H.R., Honnas, C.M., Gilleland, B.E., Barrett, M.F., Moore, J.N. and Cohen, N.D. 2023. A randomized, self-controlled case series evaluating core osteostixis of osseous cyst-like lesions of the navicular bone to improve lameness in horses with podotrochlear syndrome. Vet. Med. Res. Rep. 14, 35–46. Buchner, H.H.F., Savelberg, H.H.C.M., Schamhardt, H.C. and Barneveld, A. 1996. Limb movement adaptations in horses with experimentally induced fore- or hindlimb lameness. Equine Vet. J. 28, 63–70. Busoni, V., Heimann, M., Trenteseaux, J., Snaps, F. and Dondelinger, R.F. 2005. Magnetic resonance imaging findings in the equine deep digital flexor tendon and distal sesamoid bone in advanced navicular disease—an ex vivo study. Vet. Radiol. Ultrasound 46, 279–286. Colles, C.M. 2011. Navicular bone fractures in the horse. Equine Vet. Educ. 23, 255–261. Colles, C.M. 2001. How to repair navicular bone fractures in the horse. Proc. Am. Assoc. Equine Pract. 47, 270–278. Daniel, A.J., Goodrich, L.R., Barrett, M.F., Werpy, N.M., Morley, P.S. and McIlwraith, C.W. 2016. An optimised injection technique for the navicular bursa that avoids the deep digital flexor tendon. Equine Vet. J. 48, 159–164. Dyson, S. 2015. Navicular disease and injuries of the podotrochlear apparatus. In Robinson’s current therapy in equine medicine, 7th ed. Eds., Sprayberry, K. and Robinson, N.E. Philadelphia, PA: Saunders, pp: 856–861. Dyson, S. and Murray, R. 2007. Magnetic resonance imaging evaluation of 264 horses with foot pain: the podotrochlear apparatus, deep digital flexor tendon and collateral ligaments of the distal interphalangeal joint. Equine Vet. J. 39, 340–343. Dyson, S., Murray, R., Schramme, M. and Blunden, T. 2011. Current concepts of navicular disease. Equine Vet. Educ. 23, 27–39. Dyson, S., Murray, R., Schramme, M. and Branch, M. 2003. Lameness in 46 horses associated with deep digital flexor tendonitis in the digit: diagnosis confirmed with magnetic resonance imaging. Equine Vet. J. 35, 681–690. Dyson, S.J., Murray, R. and Schramme, M.C. 2005. Lameness associated with foot pain: results of magnetic resonance imaging in 199 horses (January 2001-December 2003) and response to treatment. Equine Vet. J. 37, 113–121. Froydenlund, T.J., Meehan, L.J., Morrison, L.R. and Labens, R. 2017. A rare case of deep digital flexor tendinopathy following centesis of the navicular bursa. Front. Vet. Sci. 4, 169. Gutierrez-Nibeyro, S.D., Werpy, N.M., White, N.A., Mitchell, M.A., Edwards, R.B., Mitchell, R.D., Gold, S.J. and Allen, A.K. 2015. Outcome of palmar/plantar digital neurectomy in horses with foot pain evaluated with magnetic resonance imaging: 50 cases (2005-2011). Equine Vet. J. 47, 160–164. Hoegaerts, M., Pille, F., De Clercq, T., Fulton, I.C. and Saunders, J.H. 2005. Comminuted fracture of the distal sesamoid bone and distal rupture of the deep digital flexor tendon. Vet. Radiol. Ultrasound 46, 234–237. Jackman, B., Baxter, G.M., Doran, R.E., Allen, D. and Parks, A. 1993. Palmar digital neurectomy in horses 57 cases (1984–1990). Vet. Surg. 22, 285–288. Kaser-Hotz, B., Ueltschi, G. and Hess, N. 1991a. Navicular bone fracture in the pelvic limb in two horses. Vet. Radiol. 32, 283–285. Kaser-Hotz, B., Ueltschi, G. and Hess, N. 1991b. Navicular bone fracture in the pelvic limb in two horses. Vet. Radiol. 32, 283–285. Lawson, S.E.M., Chateau, H., Pourcelot, P., Denoix, J.M. and Crevier-Denoix, N. 2007. Effect of toe and heel elevation on calculated tendon strains in the horse and the influence of the proximal interphalangeal joint. J. Anat. 210, 583–591. Maher, M.C., Werpy, N.M., Goodrich, L.R. and Mcilwraith, C.W. 2011. Positive contrast magnetic resonance bursography for assessment of the navicular bursa and surrounding soft tissues. Vet. Radiol. Ultrasound. 52, 385–393. Maher, O., Davis, D.M., Drake, C., Myhre, G.D., Labbe, K.M., Han, J.H. and Lejeune, S.S. 2008. Pull-through technique for palmar digital neurectomy: forty-one horses (1998–2004). Vet. Surg. 37, 87–93. Matthews, S., Dart, A.J. and Dowling, B.A. 2003. Palmar digital neurectomy in 24 horses using the guillotine technique. Aust. Vet. J. 81, 402–405. Moorman, V.J., Reiser, R.F., Mahaffey, C.A., Peterson, M.L., McIlwraith, W. and Kawcak, C.E. 2014. Use of an inertial measurement unit to assess the effect of forelimb lameness on threedimensional hoof orientation in horses at a walk and trot. Am. J. Vet. Res. 75, 800–808. Moorman, V.J., Reiser, R.F., Peterson, M.L., McIlwraith, C.W. and Kawcak, C.E. 2013. Effect of forelimb lameness on hoof kinematics of horses at a walk. Am. J. Vet. Res. 74, 1192–1197. Németh, F. and Goedegebuure, S.A.D. Von Strahlbeinfrakturen beim Pferd. In 8 Arbeitstagung der Fachgruppe Pferdekrankheiten, 1982, Freiburg, Gießen, pp: 38–40. Németh, F. and Dik, K.J. 1985. Lag screw fixation of sagittal navicular bone fractures in five horses. Equine Vet. J. 17, 137–139. Piccot-Crézollet, C., Cauvin, E.R. and Lepage, O.M. 2005. Comparison of two techniques for injection of the podotrochlear bursa in horses. J. Am. Vet. Med. Assoc. 226, 1524–1528. Rose, R.J. 1977. Bilateral luxation of the coffin joints in a horse, as a sequel to palmar neurectomy. Vet. Rec. 100, 198–199. Sampson, S.N., Schnieder, R.K., Gavin, P.R., Ho, C.P., Tucker, R.L. and Charles, E.M. 2009. Magnetic resonance imaging findings in horses with recent onset navicular syndrome but without radiographic abnormalities. Vet. Radiol. Ultrasound 50, 339–346. Schoonover, M.J., Jann, H.W. and Blaik, M.A. 2005. Quantitative comparison of three commonly used treatments for navicular syndrome in horses. Am. J. Vet. Res. 66, 1247–1251. Schramme, M.C., Boswell, J.C., Hamhougias, K., Toulson, K. and Viitanen, M. 2000. An in vitro study to compare 5 different techniques for injection of the navicular bursa in the horse. Equine Vet. J. 32, 263–267. Serra Bragança, F.M., Hernlund, E., Thomsen, M.H., Waldern, N.M., Rhodin, M., Byström, A., van Weeren, P.R. and Weishaupt, M.A. 2021. Adaptation strategies of horses with induced forelimb lameness walking on a treadmill. Equine Vet. J. 53, 600–611. Waguespack, R.W. and Hanson, R.R. 2011. Treating navicular syndrome in equine patients. Compend. Contin. Educ. Vet. 33, E2. Waguespack, R.W. and Hanson, R.R. 2010. Navicular syndrome in equine patients: anatomy, causes, and diagnosis. Compend. Contin. Educ. Vet. 32, E7. Weishaupt, M.A., Wiestner, T., Hogg, H.P., Jordan, P. and Auer, J.A. 2006. Compensatory load redistribution of horses with induced weight-bearing forelimb lameness trotting on a treadmill. Vet. J. 171, 135–146. Whitcomb, M.B. 2008. Ultrasonographic appearance and distribution of deep digital flexor injuries in the pastern region. Proc. Am. Assoc. Equine Pract. 54, 452–454. Whitcomb, M.B. 2005. How to perform a complete ultrasonographic evaluation of the pastern. Proc. Am. Assoc. Equine Pract. 51, 465–472. Zubrod, C.J. and Barrett, M.F. 2007. Magnetic resonance imaging of tendon and ligament injuries. Clin. Tech. Equine Pract. 6, 217–229. | ||
| How to Cite this Article |
| Pubmed Style Larsen EA, Williams MR, Schoonover MJ, Jurek KA, Young JM, Duddy HR. Navicular bone fracture and severe deep digital flexor tendinopathy after palmar digital neurectomy in two horses. Open Vet. J.. 2023; 13(12): 1752-1759. doi:10.5455/OVJ.2023.v13.i12.24 Web Style Larsen EA, Williams MR, Schoonover MJ, Jurek KA, Young JM, Duddy HR. Navicular bone fracture and severe deep digital flexor tendinopathy after palmar digital neurectomy in two horses. https://www.openveterinaryjournal.com/?mno=167836 [Access: January 22, 2026]. doi:10.5455/OVJ.2023.v13.i12.24 AMA (American Medical Association) Style Larsen EA, Williams MR, Schoonover MJ, Jurek KA, Young JM, Duddy HR. Navicular bone fracture and severe deep digital flexor tendinopathy after palmar digital neurectomy in two horses. Open Vet. J.. 2023; 13(12): 1752-1759. doi:10.5455/OVJ.2023.v13.i12.24 Vancouver/ICMJE Style Larsen EA, Williams MR, Schoonover MJ, Jurek KA, Young JM, Duddy HR. Navicular bone fracture and severe deep digital flexor tendinopathy after palmar digital neurectomy in two horses. Open Vet. J.. (2023), [cited January 22, 2026]; 13(12): 1752-1759. doi:10.5455/OVJ.2023.v13.i12.24 Harvard Style Larsen, E. A., Williams, . M. R., Schoonover, . M. J., Jurek, . K. A., Young, . J. M. & Duddy, . H. R. (2023) Navicular bone fracture and severe deep digital flexor tendinopathy after palmar digital neurectomy in two horses. Open Vet. J., 13 (12), 1752-1759. doi:10.5455/OVJ.2023.v13.i12.24 Turabian Style Larsen, Elizabeth A., Megan R. Williams, Mike J. Schoonover, Kelsey A. Jurek, Jenna M. Young, and Hugh R. Duddy. 2023. Navicular bone fracture and severe deep digital flexor tendinopathy after palmar digital neurectomy in two horses. Open Veterinary Journal, 13 (12), 1752-1759. doi:10.5455/OVJ.2023.v13.i12.24 Chicago Style Larsen, Elizabeth A., Megan R. Williams, Mike J. Schoonover, Kelsey A. Jurek, Jenna M. Young, and Hugh R. Duddy. "Navicular bone fracture and severe deep digital flexor tendinopathy after palmar digital neurectomy in two horses." Open Veterinary Journal 13 (2023), 1752-1759. doi:10.5455/OVJ.2023.v13.i12.24 MLA (The Modern Language Association) Style Larsen, Elizabeth A., Megan R. Williams, Mike J. Schoonover, Kelsey A. Jurek, Jenna M. Young, and Hugh R. Duddy. "Navicular bone fracture and severe deep digital flexor tendinopathy after palmar digital neurectomy in two horses." Open Veterinary Journal 13.12 (2023), 1752-1759. Print. doi:10.5455/OVJ.2023.v13.i12.24 APA (American Psychological Association) Style Larsen, E. A., Williams, . M. R., Schoonover, . M. J., Jurek, . K. A., Young, . J. M. & Duddy, . H. R. (2023) Navicular bone fracture and severe deep digital flexor tendinopathy after palmar digital neurectomy in two horses. Open Veterinary Journal, 13 (12), 1752-1759. doi:10.5455/OVJ.2023.v13.i12.24 |