| Original Article | ||
Open Vet J. 2022; 12(3): 335-340 Open Veterinary Journal, (2022), Vol. 12(3): 335–340 Original Research Novel Achilles tendon repair technique utilizing an allograft and hybrid external fixator in dogsSamuel J. Tidwell1, Ken Greenwood2 and Samuel P. Franklin1*1Colorado Canine Orthopedics, Colorado Springs, CO, USA 2Northlake Veterinary Surgery, Clarkston, GA. USA *Corresponding Author: Samuel P. Franklin. Kansas City Canine Orthopedics, West Shawnee, KS, USA.Email: sam17franklin [at] hotmail.com Submitted: 06/01/2022 Accepted: 03/05/2022 Published: 23/05/2022 © 2022 Open Veterinary Journal
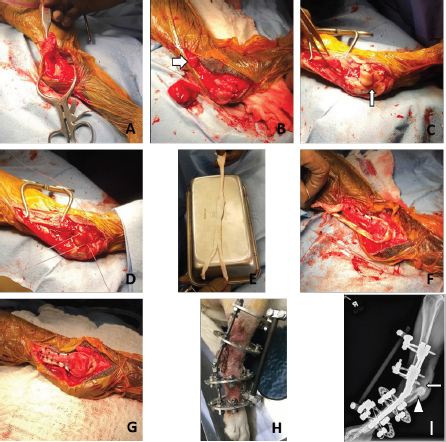
AbstractBackground: Achilles mechanism rupture is a surgical condition involving primary tenorrhaphy with various described means of surgical augmentation and bolstering. Aim: To report complications and outcomes with a novel Achilles repair technique in dogs using a superficial digital flexor tendon (SDFT) or deep digital flexor tendon (DDFT) allograft. Methods: Medical records were reviewed for dogs with chronic rupture or deterioration of the Achilles mechanism. Fibrous tissue was excised and either primary tenorrhaphy or reattachment of the tendon(s) to the calcaneus was performed. The surgical repair was supplemented by an SDFT or DDFT allograft, and postoperative immobilization was provided using a transarticular hybrid external skeletal fixator. Complications were classified as minor, major, or catastrophic, and function was classified as full, acceptable, or unacceptable, based on established guidelines. Results: Complications occurred with 6 out of 12 repairs, including 1 minor, 6 major, and 2 catastrophic complications. The two catastrophic complications were the recurrence of tarsal hyperflexion and lameness at 20 weeks and 18 months following surgery. Of the 12 surgeries performed, 2 resulted in full function, 8 with acceptable function, and 2 with unacceptable function at last follow-up 17–98 weeks postsurgery (mean=45 weeks) for a success rate of 10/12 cases. Conclusion: The use of SDFT or DDFT allografts, coupled with an external fixator, can provide a moderate rate of full or acceptable functional outcomes and appears a viable treatment. However, complications were frequent and without a comparison group no conclusions can be drawn about the inferiority or superiority of this technique to other techniques for Achilles mechanism repair in dogs. Keywords: Achilles tendon, Allograft, Common calcaneal tendon, Dog, Transplantation. IntroductionMultiple surgical techniques have been described for repairing damage to the Achilles mechanism in dogs. The most common technique involves simple tenorrhaphy at the location of tendon injury, including reattachment to the calcaneus if injury is at this location, followed by tarsal immobilization (Worth et al., 2004; Nielsen and Pluhar, 2006; Corr et al., 2010; Schulz et al., 2019). Reported success rates with such treatment are generally good, but can be as low as 70% (Worth et al., 2004; Nielsen and Pluhar, 2006; Corr et al., 2010; Schulz et al., 2019). Accordingly, numerous reports detail addition of materials to try and support the tenorrhaphy including the use of an “artificial” tendon (Morton et al., 2015; Buttin et al., 2020), mesh (Gall et al., 2009), bone plates (Zellner et al., 2018), muscle grafts (Baltzer and Rist, 2009), the flexor digitorum lateralis tendon (Katayama, 2016), and tensor fascia lata autografts (Shani and Shahar, 2000). Success has been reported with most of these augmented techniques (Shani and Shahar, 2000; Baltzer and Rist, 2009; Gall et al., 2009; Morton et al., 2015; Katayama, 2016; Zellner et al., 2018; Buttin et al., 2020), but each has its drawbacks. Repairs with artificial materials pose concern for potential infection and the need for subsequent removal, while autologous tissue harvest potentially creates additional morbidity. As an alternative to the aforementioned materials, allograft tendons are sometimes used in people when there is a large defect or the native Achilles tendon has deteriorated substantially (Song and Hua, 2019). These allogeneic grafts are biological materials that can be colonized by native cells and integrate with surrounding tissue, a potential benefit over synthetic implants (Nellas et al., 1996; Song and Hua, 2019). In comparison with autograft tendons, allograft tendons are appealing due to off-the-shelf availability, lack of morbidity associated with autologous tissue harvest, and desirable mechanical strength of the allograft (Nellas et al., 1996; Song and Hua, 2019). Furthermore, lyophilization and decellularization of the allograft decrease the immunogenicity and typically render it well tolerated by the recipient (Song and Hua, 2019). Allogeneic tendons or fascia have also been used for a number of purposes in veterinary patients. Specifically, in one study, allogeneic tensor fascia lata grafts were used for perineal hernia repair, repair of urethral defects, periodontal surgery, and to support tenorrhaphy of a ruptured Achilles mechanism (El-Taliawi et al., 2020). In another study, deep digital flexor tendon (DDFT) allografts were used for intra-articular reconstruction of ruptured cranial cruciate ligaments in dogs with success in some patients (Biskup et al., 2017). Two other studies report on four dogs with flexor carpi ulnaris, patella tendon, or Achilles mechanism repair (n=2 dogs) supplemented with an Achilles tendon allograft (Alam et al., 2013; Serra et al., 2020). No evidence of disease transmission or immune rejection was noted with allograft application in any of these patients. Given the appealing features of an allograft, its application may be a viable method of supporting treatment of Achilles mechanism ruptures in dogs. However, there are also potential downsides to the use of allograft transplantation, including added cost, increased complexity of the surgery, and risk of disease transmission or an immunologic response. As a result, the decision to use, or not use, an allograft should include consideration of the pros and cons of allograft use and would ideally be based upon clinically relevant data. The purpose of this study was to retrospectively report complications and outcomes of Achilles mechanism repairs in dogs that were supplemented with the use of an SDFT or DDFT allograft and protected with a hybrid external skeletal fixator (ESF). Materials and MethodsThis was a retrospective study and included dogs with repair of a chronic Achilles mechanism injury or deterioration between March 2019 and March 2021. Included dogs could have complete rupture of the gastrocnemius tendon, the superficial digital flexor tendon, or the common tendon of the biceps femoris, semitendinosus, and gracilis, which we will refer to as the common tendon, or any combination thereof. Surgical outcomes were established by physical examination, or review of videos, with owner input. Definitions of outcome and complications were based on previously proposed criteria (Cook et al, 2010). Briefly, functional outcomes were considered full, if the dog returned to pre-injury status without the need for medications, acceptable, if pre-injury status was obtained but limited in level or duration or required the use of medication, or unacceptable, which includes all other outcomes. Complications were classified as minor if no treatment were performed, major, if any treatment whether medical or surgical were provided, and catastrophic, if it caused permanent unacceptable function. Success was defined as obtaining full or acceptable function. Surgical techniqueIn those dogs that had chronic degeneration or rupture of the gastrocnemius and common tendons with an intact superficial digital flexor tendon, the surgical approach included isolating and reflecting the native superficial digital flexor tendon to access the gastrocnemius and common tendons (Fig. 1). Resection of a portion of the abnormal gastrocnemius and common tendons was then performed (Fig. 1). The amount of tissue excised was determined subjectively, but was guided by the goal to remove as much grossly abnormal tissue as possible while retaining enough native tendon(s) so that it could be reattached to the calcaneus with the stifle extended and the tarsus mildly flexed. After removing the abnormal tendinous tissue, a notch was created using a burr on the plantar aspect of the calcaneus about 7–10 mm distal to the tuberosity, into which the allograft tendon would eventually be placed (Fig. 1). Two slightly divergent bone tunnels, each 2.0 mm in diameter) were then drilled from the proximal calcaneal tuberosity to exit the proximal and abaxial portion of the burred notch. The native gastrocnemius and common tendon were then reattached to the calcaneus using #2 FiberWire (Arthrex Vet Systems, Naples, FL) placed through the two tunnels in the calcaneus and using a double Krackow suture pattern (Fig. 1). The allograft was then applied to bolster the surgical repair. The graft was first trimmed to be just narrow enough to be placed into the burred notch in the calcaneus; a 5–6 mm width was commonly desired (Fig. 1). The allogeneic graft was then sutured along one side of the gastrocnemius tendon, wrapped down around the calcaneus and placed in the burred notch on the plantar aspect of the calcaneus (Fig. 1), and sutured under tension along the contralateral side of the gastrocnemius tendon in a U-shape (Fig. 1). Polypropylene and/or polydioxanone were used in a simple interrupted or simple continuous pattern to secure the allograft to the native gastrocnemius/common tendons. Closure involved replacing the native SDFT to its normal position and suturing it into place using polypropylene or polydioxanone. The remaining closure was routine. In the one patient that had a chronic mid-tendon laceration/rupture of all components of the Achilles mechanism, surgery involved debriding fibrous tissue and reapposing the ruptured tendon ends with a 3-loop pulley using #5 FiberWire (Arthrex, Naples, FL). An SDFT allograft was then placed over the caudal aspect of the tenorrhaphy and secured both proximal and distal to the tenorrhaphy using interrupted sutures of polydioxanone (Fig. 1). Following closure, in all cases a hybrid external skeletal fixator was applied. All ESFs included a double-ring block, typically using 66 mm diameter rings, distal to the tarsus with four tensioned wires. A double-ring block of two partial rings, or one partial and one complete ring, was secured to the tibia with three or four ESF half-pins inserted into the cranial or medial aspect of the tibia (Fig. 1). The ring blocks were joined by threaded rods and one hinge each on the medial and lateral side of tarsus. The hinges were locked (no motion). An additional connecting bar was secured to the cranial aspect of the most proximal and most distal rings to buttress the fixator and prevent any undesired tarsal flexion. The ESF maintained the tarsus between approximately 140–150 degrees of tarsal extension. A bandage was applied around the ESF with 4 × 4 gauze sponges, wetted with approximately 0.05% chlorhexidine, applied at the pin–skin interfaces. All dogs were discharged with an oral nonsteroidal anti-inflammatory medication to be used for 14 days, Cephalexin (22 mg/kg TID) for 10 days, and a sedative (Acepromazine 0.5–1 mg/kg up to ITD) to be used as needed. Bandage changes were recommended to be performed twice in the first week following surgery and then weekly thereafter until the pin tracts had healed, typically around 4 weeks postsurgery. During this time, the dogs were allowed to go on leash walks that started with 5 minutes duration but progressed to 15–20 minutes duration (1–2 such walks per day maximum with additional brief walks) during the second month of care. All patients were maintained in the ESF for 8–10 weeks postsurgery. Following ESF removal, owners were advised to perform extensive leash activity for 1 to 2 additional months and then begin resuming off leash activity.
Fig. 1. (A) Gastrocnemius and common tendon severed. (B) Abnormal gastrocnemius and common tendon excision; normal tendon tissue indicated by arrow. (C) Plantar calcaneal notch burred. (D) Double Krackow suture pattern used to reattach gastrocnemius and common tendon through two calcaneal tunnels. (E) SDFT allograft. (F) Allograft sutured to one side and tension applied. (G) Allograft sutured to medial and lateral sides of the native gastrocnemius tendon. Note that additional interrupted sutures were placed to secure the allograft to the native gastrocnemius tendon prior to surgical closure. (H) Hybrid external skeletal fixator (ESF) applied. (I) Postoperative radiograph; the drill tunnels from the proximal tuber to the plantar calcaneal notch are indicated by the arrow and the plantar calcaneal notch is indicated by a triangle. Ethical approvalAll clients provided informed, written consent for treatment of their dogs. As this was a retrospective case series, no ethical approval was required for the study. ResultsThere were 12 surgical repairs of chronic ruptures/deteriorations in 11 dogs that were supported with an allograft and thus included in this report. There were eight spayed females, one intact female, one neutered male, and one intact male. Age ranged from 2 to 11 years (mean=7.1 ± 2.5) and weight ranged from 21.3 to 48.2 kg (mean=29.9 ± 8.0). Follow-up time ranged from 17 to 98 weeks (mean=44.9 ± 24.4). Ten dogs had chronic degeneration of the gastrocnemius and common tendon at their insertion on the calcaneus with an intact native SDFT. One of these dogs had bilateral repairs staged 16 weeks apart (i.e., 11 surgical repairs of chronic gastrocnemius/common tendon degeneration with an intact native SDFT). Ten of these 11 repairs were bolstered with an SDFT allograft and one was bolstered with a DDFT allograft because no SDFT graft was available. One additional dog had a chronic (3-week-old) complete laceration of the Achilles mechanism at the mid-tendon level. This patient had primary tenorrhaphy supported with an SDFT allograft. Of the 12 surgeries performed, 2 repairs resulted in full function, 8 with acceptable function, and 2 with unacceptable function for a success rate of 10/12 cases. The one dog with a 3-week old mid-tendon laceration obtained full functional outcome. Nine of 11 repairs in dogs with chronic gastrocnemius and common tendon deterioration at the calcaneal insertion achieved acceptable or full function with 2 dogs having an unacceptable final outcome. Complications were encountered with 6 of 12 repairs, including 1 minor, 6 major, and 2 catastrophic complications (1 repair had 2 complications and one had 3 complications). One dog was suspected to have a ruptured part of the native superficial digital flexor tendon distal and plantar to the tuber calcaneus in the region of the allograft. This dog developed hyperextension of the digits 28 weeks postsurgery. The dog remained strongly ambulatory without tarsal hyperflexion and no development of sores on any of the pads of the pes. No treatment was provided and the patient continued to have acceptable function 44 weeks postsurgery. Based on strict application of the complication definitions, this was classified as a minor complication. There were two major complications associated with the ESF. One dog fractured metatarsals II–V within the first week following surgery at the level of the distal ESF wires. The ESF was removed and a cast was applied to stabilize the fractures and support the Achilles mechanism repair. The metatarsals healed uneventfully within 2 months of surgery and the cast was removed. That dog has acceptable function 34 weeks postsurgery. Another dog suffered a tibial fracture at the level of the proximal tibial ESF pin 7 days after Achilles repair as a result of a minor trauma. Surgery was performed to stabilize the fracture with two positional screws and extending the ESF proximal to the fracture site. The fracture healed uneventfully and the dog had acceptable function on that limb 59 weeks post-Achilles repair. Two dogs had confirmed infection and fiberwire removal. In one dog, the infection manifested within 20 weeks following surgery; the fiberwire was removed and the dog had an acceptable function 14 weeks following fiberwire removal. Another dog had a broken wire of the ESF and some evidence of infection of the Achilles repair within 10 weeks following surgery. The ESF wire was advanced to address the broken wire and antibiotics were used to address any infection. The dog achieved acceptable function and competed for several months in hunting competitions. However, at 18 months postrepair, the dog had evidence of infection again and so the fiberwire was removed. The owner reported that the final outcome, 2 months following implant removal, was that the hock was hyperflexed. No video or physical exam was performed at this time but given the owner input this patient was classified as having a catastrophic complication with an unacceptable outcome. The other catastrophic complication included recurrence of plantigrade stance in 1 dog 20 weeks following surgical repair. The cause of the plantigrade stance appeared, based on physical examination, to be at the musculotendinous junction, away from the surgical repair performed distally at the tuber calcaneus. Attempted re-repair was offered but the owners elected pantarsal arthrodesis instead. DiscussionOur subjective impression is that the success rate in this study is at least comparable if not superior to our success rates using simple repairs without any augmentation of the tenorrhaphy. This impression is tentatively supported by previous studies that cite unacceptable outcomes of up to 30% in cases without tenorrhaphy augmentation (Worth et al., 2004; Nielsen and Pluhar, 2006; Corr et al., 2010), as well as the numerous surgeons and reports that document use of tenorrhaphy augmentation (Nellas et al., 1996; Shani and Shahar, 2000; Baltzer and Rist, 2009; Alam et al., 2013; Morton et al., 2015; Katayama, 2016; Zellner et al., 2018; Schulz et al., 2019; Song and Hua, 2019; Buttin et al., 2020; El-Taliawi et al., 2020; Serra et al., 2020). Consequently, we hypothesize that bolstering the Achilles mechanism repairs is beneficial. However, we cannot definitively make that conclusion as there was no comparison group in this study, nor do we know whether use of an allograft provides superior outcomes in comparison to other methods of tendon reinforcement. We can only tentatively conclude that allograft augmentation of Achilles tendon repair appears to be one more viable option based on the functional outcomes obtained in this group of dogs. When considering whether allograft transplantation as it was applied in these dogs is a good choice, we also need to consider whether there were any complications attributable to the allograft use that would suggest this technique is a poor choice. Although there was a high overall complication rate, we did not recognize any disease transmission or immune-associated rejection associated with the allograft use, consistent with previous reports of allograft use for musculoskeletal applications in dogs (Alam et al., 2013; Biskup et al., 2017; El-Taliawi et al., 2020; Serra et al., 2020). As for the potential for allografts to harbor infection, two dogs had confirmed infection but clinical signs of infection resolved quickly with removal of the fiberwire and polypropylene. This leads us to conclude that removal of the allograft itself will not be necessary, and that bacteria were more likely harbored on the braided suture material rather than the allograft. Consequently, we tentatively conclude that an allograft is likely safe from an infectious disease standpoint. The other complication that could potentially have been attributable to the allograft was the possible rupture of the superficial digital flexor tendons on the plantar aspect of the calcaneus, leading to hyperextended digits in one dog. Although this dog did well clinically, this finding is of concern. While we do not have a definitive explanation for this finding, we tentatively conclude that the allograft tendon, as well as the knots for the primary tenorrhaphy, should be adequately recessed into the burred notch on the plantar aspect of the calcaneus so as to not pose a risk of abrading the native superficial digital flexor tendon. The additional complications in this case series were all attributable to the external skeletal fixator. This finding that complications are commonly associated with the post-op immobilization was identified in another study of Achilles mechanism repair as well (Nielsen and Pluhar, 2006). We had chosen an ESF in an effort to provide dogs with greater mobility than that afforded by external coaptation. Indeed, many of the dogs were quite mobile in their fixators walking up to 40 minutes a day. Given that application of an ESF has been shown to allow substantial strain on the Achilles (Lister et al., 2009), but presumably without elongation of the repair, the repetitive isometric strain enabled by use of an ESF may have been beneficial to tendon healing and contributed to those cases with positive outcomes achieved in this study. Conversely, a recent cadaver study, albeit with a different type of ESF, did not find a mechanical advantage of ESF over external coaptation (Sugiyama et al., 2018). Therefore, given the complications suffered with the ESF, and the time and expense associated with ESF use, we question whether use of external coaptation would be equally efficacious, easier, less expensive, less risky for fracture, and therefore a more prudent choice. The data in this study do not allow us to answer that question effectively. This study has several notable limitations in addition to the fact that it was retrospective in nature without a comparison group. Notably, there were numerous attributes of the surgical and postoperative care that could have affected outcomes, including the addition of the allograft in comparison to either no bolstering of the surgical repair or use of some other support. Similarly, both the suture type and suture technique for the primary tenorrhaphy may affect outcomes. Finally, post-op immobilization techniques and postsurgical procedures may also impact outcomes. As a result of all these confounding factors, we can only conclude that this novel technique as a whole can be used with success, but also had high complication rates. We do not know if this technique is superior to any other treatment options and we do not know which components of this technique are relevant in providing success, or which could be omitted. Further study and technique development is warranted to achieve consistent success with lower complication rates. However, we do conclude that use of the allograft as applied in this study, coupled with an external fixator, is a viable option that can be justifiably applied in clinical practice. AcknowledgmentsThe authors thank Dr. Gary Brown for teaching them this technique and they thank Dr. Gary Anderson for providing valuable postoperative care for one of the patients. Conflict of interestNo proprietary or conflict of interest for this project. Authors’ contributionsS.J. Tidwell assisted with data collection and evaluation and drafted and revised the final manuscript. S.P. Franklin conceived of the study design, performed the surgeries, assisted with data collection and evaluation, and assisted with and revised the final manuscript. K. Greenwood originally described the reported surgical technique to S.P. Franklin and reviewed the final manuscript. ReferencesAlam, M.R., Gordon, W.J., Heo, S.Y., Lee, K.C., Kim, N.S., Kim, M.S. and Lee, H.B. 2013. Augmentation of ruptured tendon using fresh frozen Achilles tendon allograft in two dogs; a Case Report. Vet. Med. 58, 50–55. Baltzer, W.I. and Rist, P. 2009. Achilles tendon repair in dogs using the semitendinosus muscle: surgical technique and short-term outcome in five dogs. Vet. Surg. 38, 770–779. Biskup, J.J., Balogh, D.G., Scott, R.M. and Conzemius, M.G. 2017. Long-term outcome of an intra-articular allograft technique for treatment of spontaneous cranial cruciate ligament rupture in the dog. Vet. Surg. 46, 691–699. Buttin, P., Goin, B., Cachon, T. and Viguier, E. 2020. Repair of Tendon Disruption Using a Novel Synthetic Fiber Implant in Dogs and Cats: The Surgical Procedure and Three Case Reports. Vet. Med. Intl. 2020, 1–9. Cook, J.L., Evans, R., Conzemius, M.G., Duncan, B., Lascelles, B.D., McIlwraith, C.W., Pozzi, A., Clegg, P., Innes, J., Schulz, K., Houlton, J., Fortier, L., Cross, A.R., Hayashi, K., Kapatkin, A., Brown, D.C. and Stewart, A. 2010. Proposed definitions and criteria for reporting time frame, outcome, and complications for clinical orthopedic studies in veterinary medicine. Vet. Surg. 39, 905–908. Corr, S.A., Draffan, D., Kulendra, E., Carmichael, S. and Brodbelt, D. 2010. Retrospective study of Achilles mechanism disruption in 45 dogs. Vet. Rec. 167, 407–411. El-Taliawi, O.G., Taguchi, T., Dong, F., Battig, J. and Griffon, D.J. 2020. Biocompatibility of allogeneic canine fascia lata: In vitro evaluation and small case series. Vet. Surg. 49, 310–320. Gall, T.T., Santoni, B.G., Egger, E.L., Puttlitz, C.M. and Rooney, M.B. 2009. In vitro biomechanical comparison of polypropylene mesh, modified three-loop pulley suture pattern, and a combination for repair of distal canine achilles’ tendon injuries. Vet. Surg. 38, 845–851. Katayama, M. 2016. Augmented repair of an achilles tendon rupture using the flexor digitorum lateralis tendon in a toy poodle. Vet. Surg. 45, 1083–1086. Lister, S.A., Renberg, W.C. and Roush, J.K. 2009. Efficacy of immobilization of the tarsal joint to alleviate strain on the common calcaneal tendon in dogs. Am. J. Vet. Res. 70, 134–140. Morton, M.A., Thomson, D.G., Rayward, R.M., Jiménez-Peláez, M. and Whitelock, R.G. 2015. Repair of chronic rupture of the insertion of the gastrocnemius tendon in the dog using a polyethylene terephthalate implant. Vet. Comp. Orthop. Traumatol. 28, 282–287. Nellas, Z.J., Loder, B.G. and Wertheimer, S.J. 1996. Reconstruction of an Achilles tendon defect utilizing an Achilles tendon allograft. J. Foot Ankle Surg. 35, 144–148. Nielsen, C. and Pluhar, G.E. 2006. Outcome following surgical repair of Achilles tendon rupture and comparison between postoperative tibiotarsal immobilization methods in dogs. Vet. Comp. Orthop. Traumatol. 19, 246–249. Schulz, K.S., Ash, K.J. and Cook, J.L. 2019. Clinical outcomes after common calcaneal tendon rupture repair in dogs with a loop-suture tenorrhaphy technique and autogenous leukoreduced platelet-rich plasma. Vet. Surg. 48, 1262–1270. Serra, C.I., Navarro, P., Guillem, R. and Soler, C. 2020. Use of frozen tendon allograft in two clinical cases: Common Calcaneal Tendon and Patellar Ligament Rupture. J. Am. Anim. Hosp. Assoc. 56, 315–319. Shani, J. and Shahar, R. 2000. Repair of chronic complete traumatic rupture of the common calcaneal tendon in a dog, using a fascia lata graft. Vet. Comp. Orthop. Traumatol. 13, 104–108. Song, Y.J. and Hua, Y.H. 2019. Tendon allograft for treatment of chronic Achilles tendon rupture: a systematic review. J. Foot Ankle Surg. 25, 252–257. Sugiyama, T., Woodward, A. and Ryan, S.D. 2018. Biomechanical evaluation of 6 transarticular tibiotarsal immobilization methods in canine cadaveric limbs. Vet. Surg. 47, 705–714. Worth, A.J., Danielsson, F., Bray, J.P., Burbidge, H.M. and Bruce, W.J. 2004. Ability to work and owner satisfaction following surgical repair of common calcanean tendon injuries in working dogs in New Zealand. N. Z. Vet. J. 52, 109–116. Zellner, E.M., Hale, M.J. and Kraus, K.H. 2018. Application of tendon plating to manage failed calcaneal tendon repairs in a dog. Vet. Surg. 47, 439–444. | ||
| How to Cite this Article |
| Pubmed Style Tidwell SJ, Greenwood K, Franklin SP. Novel Achilles Tendon Repair Technique Utilizing an Allograft and Hybrid External Fixator in Dogs. Open Vet J. 2022; 12(3): 335-340. doi:10.5455/OVJ.2022.v12.i3.5 Web Style Tidwell SJ, Greenwood K, Franklin SP. Novel Achilles Tendon Repair Technique Utilizing an Allograft and Hybrid External Fixator in Dogs. https://www.openveterinaryjournal.com/?mno=139835 [Access: April 20, 2024]. doi:10.5455/OVJ.2022.v12.i3.5 AMA (American Medical Association) Style Tidwell SJ, Greenwood K, Franklin SP. Novel Achilles Tendon Repair Technique Utilizing an Allograft and Hybrid External Fixator in Dogs. Open Vet J. 2022; 12(3): 335-340. doi:10.5455/OVJ.2022.v12.i3.5 Vancouver/ICMJE Style Tidwell SJ, Greenwood K, Franklin SP. Novel Achilles Tendon Repair Technique Utilizing an Allograft and Hybrid External Fixator in Dogs. Open Vet J. (2022), [cited April 20, 2024]; 12(3): 335-340. doi:10.5455/OVJ.2022.v12.i3.5 Harvard Style Tidwell, S. J., Greenwood, . K. & Franklin, . S. P. (2022) Novel Achilles Tendon Repair Technique Utilizing an Allograft and Hybrid External Fixator in Dogs. Open Vet J, 12 (3), 335-340. doi:10.5455/OVJ.2022.v12.i3.5 Turabian Style Tidwell, Samuel J, Ken Greenwood, and Samuel P Franklin. 2022. Novel Achilles Tendon Repair Technique Utilizing an Allograft and Hybrid External Fixator in Dogs. Open Veterinary Journal, 12 (3), 335-340. doi:10.5455/OVJ.2022.v12.i3.5 Chicago Style Tidwell, Samuel J, Ken Greenwood, and Samuel P Franklin. "Novel Achilles Tendon Repair Technique Utilizing an Allograft and Hybrid External Fixator in Dogs." Open Veterinary Journal 12 (2022), 335-340. doi:10.5455/OVJ.2022.v12.i3.5 MLA (The Modern Language Association) Style Tidwell, Samuel J, Ken Greenwood, and Samuel P Franklin. "Novel Achilles Tendon Repair Technique Utilizing an Allograft and Hybrid External Fixator in Dogs." Open Veterinary Journal 12.3 (2022), 335-340. Print. doi:10.5455/OVJ.2022.v12.i3.5 APA (American Psychological Association) Style Tidwell, S. J., Greenwood, . K. & Franklin, . S. P. (2022) Novel Achilles Tendon Repair Technique Utilizing an Allograft and Hybrid External Fixator in Dogs. Open Veterinary Journal, 12 (3), 335-340. doi:10.5455/OVJ.2022.v12.i3.5 |