| Original Article | ||
Open Vet J. 2022; 12(1): 105-113 Open Veterinary Journal, (2022), Vol. 12(1): 105–113 Original Research The relationship between urethral sphincter mechanism incompetency and lower back pain: Positing a novel treatment for urinary incontinence in dogsDavid M. Lane1*, and Sarah A. Hill21Points East West Veterinary Services, Squamish, British Columbia, Canada 2Department of Military Psychology and Leadership, Royal Military College of Canada, Kingston, Ontario, Canada *Corresponding Author: David M. Lane. Points East West Veterinary Services, Squamish, British Columbia, Canada. Email: dlane [at] pointseastwest.com Submitted: 08/11/2021 Accepted: 27/01/2022 Published: 13/02/2022 © 2022 Open Veterinary Journal
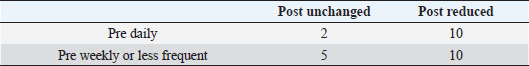
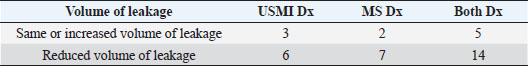
AbstractBackground: In humans, multiple researchers have not only determined that there is a relationship between urinary incontinence (UI) and lower back pain (LBP), but that by treating the LBP, clinicians are able to improve or resolve the UI. Up until now, no equivalent canine research has investigated whether treatment of LBP can improve the clinical signs of acquired, non-neurologic UI in dogs. Aim: To determine if a relationship exists between LBP and urethral sphincter mechanism incompetence (USMI) in dogs. Methods: Review of medical records of all patients that presented to Points East West Veterinary Services with a history of naturally occurring acquired UI from May 2013 to December 2019. Thirty-nine patients treated for LBP using combined acupuncture and manual therapy, and 33/39 patients that also received concurrent photobiomodulation (PBM) therapy, qualified for this study. Results: Treated patients showed a statistically significant reduction in both the frequency (p < 0.01) and volume (p < 0.01) of UI episodes. Treatment responses ranged from no improvement, to complete resolution of the USMI clinical signs. Conclusion: The reduction of USMI clinical signs following LBP treatment suggests a relationship between these two conditions. Combined acupuncture, manual therapy, with or without PBM was shown to be an effective treatment for USMI. By corollary, USMI incontinence should be considered a potential pain symptom. Keywords: Incontinence, Manual therapy, Acupuncture, Photobiomodulation, Back pain. IntrodctionUrethral sphincter mechanism incompetency (USMI) is the most common non-neurogenic acquired cause of urinary incontinence (UI) in dogs (Chew et al., 2011; Byron et al., 2017). It has a reported prevalence in spayed females ranging from 3% to 5%, with earlier research reporting it to be as high as 20% overall, and 30% in large dogs (Coit et al., 2008; Chew et al., 2011; Reichler and Hubler, 2014; Byron et al., 2017; Hall et al., 2019). The incidence of USMI in intact females, and both intact or neutered male dogs, is much lower at approximately 1% (Coit et al., 2008; Reichler and Hubler, 2014; Hall et al., 2019). USMI most commonly presents as urinary leakage while the dog is sleeping or lying down (Chew et al., 2011). The underlying physiology of USMI is uncertain, but appears to be a multifactorial condition with anatomic, genetic, neurologic, and endocrine components (Spain et al., 2004; de Bleser et al., 2011; Byron et al., 2017; Pegram et al., 2019). Research into a connection between the age of gonadectomy and prevalence of USMI has produced conflicting results, and remains controversial (Aaron et al., 1996; Thrusfield et al., 1998; Spain et al., 2004; de Bleser et al., 2011; Forsee et al., 2013; Byron et al., 2017; Hall et al., 2019; Pegram et al., 2019). In females, USMI occurs more frequently in larger dogs, with certain breeds overrepresented (Aaron et al., 1996; Hoelzler and Lidbetter, 2004; Chew et al., 2011; de Bleser et al., 2011; Forsee et al., 2013; Byron et al., 2017; Pegram et al., 2019). Other risk factors that increase the risk of USMI include having a docked tail, increased age, obesity, having a shorter urethral length, and having a bladder neck located caudally in the pelvic canal (Holt and Thrusfield, 1993; Wansbrough, 1996; Power et al., 1998; de Bleser et al., 2011; Reichler and Hubler, 2014; Hall et al., 2019; Pegram et al., 2019). De Bleser et al. (2011) also found a statistically significant correlation (p < 0.001) between USMI and both osteoarthritis (OA), and difficulty crouching. In many cases the onset of USMI does not occur until 2 to 5 years after the gonadectomy, and sometimes not until 10 years have passed (Aaron et al., 1996; Thrusfield et al., 1998; Hoelzler and Lidbetter, 2004; de Bleser et al., 2011; Forsee et al., 2013; Reichler and Hubler, 2014; Hall et al., 2019). The reason for this delay is unknown. There are conflicting findings about whether or not USMI is more prevalent in neutered versus intact males (Aaron et al., 1996; Power et al., 1998; Hall et al., 2019). Unlike USMI in females, the prevalence in males is not related to body weight (Coit et al., 2008). Histologic effects of gonadectomies on the bladder also differs between the sexes, suggesting an alternate physiologic cause (Coit et al., 2008; Hall et al., 2019). Breeds with the highest odds of incontinence are similar for both sexes (Hall et al., 2019). USMI is typically managed by eliminating the clinical signs through the long term administration of medication, with phenylpropanolamine and/or diethylstilbestrol being the most common (Hoelzler and Lidbetter, 2004; Reichler, 2009; Chew et al., 2011; Reichler and Hubler, 2014). The success rate of medical treatment is higher in female dogs, relative to males (Aaron et al., 1996; Hoelzler and Lidbetter, 2004; Chew et al., 2011; Hall et al., 2019). Patients refractory to medical treatment are candidates for surgical intervention, with success rates as high as 80%, but with some dogs only showing temporary benefit (Aaron et al., 1996; Hoelzler and Lidbetter, 2004; Reichler, 2009; Chew et al., 2011). In human medicine, multiple researchers have identified a relationship between UI and lower back pain (LBP) (Smith et al., 2006; Zhang et al., 2006; Eliasson et al., 2008). Treatment of LBP with physiotherapy and exercises in women has also been shown to reduce UI symptoms (Ghaderi et al., 2016). On the veterinary side, one researcher found a correlation between the existence of USMI, and reduced mobility of the third to fifth lumbar vertebrae (Thude, 2015). In human medicine, LBP is divided into the categories of mechanical LBP, and non-specific lower back pain (NSLBP) (Balagué et al., 2012). NSLBP is defined as LBP “not attributable to a recognisable, known specific pathology (e.g., infection, tumour, osteoporosis, fracture, structural deformity, inflammatory disorder, radicular syndrome, or cauda equina syndrome)” (Balagué et al., 2012). NSLBP is recognized as a common condition in humans, with a lifetime prevalence as high as 84% (Balagué et al., 2012). References to NSLBP appear to be non-existent in the veterinary literature. Diagnosis of NSLBP in humans is made by a combination of pain on palpation, detection of asymmetry, and abnormal mobility of vertebral structures (Flynn et al., 2002). These diagnostic techniques have also been adapted and applied to veterinary patients (Millis and Levine, 2013; Lane and Hill, 2016a, 2016b; Zink and Van Dyke, 2018). Treatment of NSLBP in humans often includes prescription medication, manual therapy, stabilization exercises, and other specific therapeutic exercises (Zhang et al., 2006; Fritz et al., 2007; Balagué et al., 2012). These treatments are also applicable to dogs (Millis and Levine, 2013; Lane and Hill, 2016a, 2016b; Zink and Van Dyke, 2018). In humans, multiple studies have shown evidence that acupuncture can reduce the symptoms of UI and is not inferior to other more established treatments (Shen et al., 2019; Sun et al., 2020). Similarly, systematic review concluded that photobiomodulation (PBM) benefitted human UI patients (Mackova et al., 2020). In the veterinary literature, blinded, controlled, prospective, clinical trials found that combining acupuncture and manual therapy (CAMT) improved short-term comfort and mobility in dogs (Lane and Hill, 2016a, 2016b). It is unknown whether there is a relationship between LBP and USMI in dogs, the way that there appears to be between LBP and UI in people. However, if such a relationship exists, it follows that resolution of that back pain would lead to a subsequent decrease in UI. The hypothesis of this paper is that dogs treated for LBP using CAMT, with or without PBM, will demonstrate a subsequent reduction in the frequency and/or volume of UI episodes. Materials and MethodsThis retrospective study examined the medical records of patients that presented to Points East West Veterinary Services from May 2013 to December 2019. Records of patients with a reported history of UI consistent with USMI were examined for evidence of clinical improvement following treatment for concurrent LBP. Specifically, only patients with a history of acquired incontinence while sleeping or lying down, or immediately upon first rising following a period of lying down, were included. Patients with incontinence while awake and alert, or with evidence of neurologic dysfunction on physical examination, were excluded. Patients with a history of uncontrolled polyuria/polydipsia, stranguria, or dysuria, were also excluded. Because the history of UI was often learned incidentally during the initial appointment, and the first treatment was also begun during that same appointment, there was not an opportunity to perform other diagnostic tests, such as urinalysis, radiographic, or ultrasound imaging beforehand. Similarly, there was insufficient time to determine what, if any, prior diagnostic workup for UI had been performed with the patients’ regular veterinarian. Thus, because of the time constraints of clinical practice, the diagnosis of USMI was presumptive, based on the clinical history alone. The history was collected orally, by the same clinician (David Lane) for all patients. No notation was made about whether it was always the same family member reporting the clinical response during follow up inquiries. However, if the family member reporting the clinical response on subsequent appointments was not able to provide adequate information, that patient was excluded from the study. Because CAMT has previously demonstrated a benefit in comfort and mobility within 8 days of a second treatment (Lane and Hill, 2016a, 2016b), any reduction in the clinical signs of USMI that did not occur within 8 days of a second treatment, were not considered related to the treatment. All patients received at least two treatments of CAMT, with or without PBM. Patients whose clinical presentation required additional treatment beyond CAMT and PBM, were excluded from the study. Patients for whom there was insufficient data following treatment, and for whom the history of incontinence was so sporadic that the owner was unable to determine if there was a timely response to treatment, were excluded. This means that patients who were receiving pharmaceutic treatment, or that could implement husbandry practises that completely resolved the UI, were excluded. However, patients with uncontrolled UI, despite pharmaceutic or husbandry interventions, were included, as long as those interventions did not change while the success of treatment was being evaluated. Information was tabulated on the patients’ signalment, clinical history, physical examination findings, clinical outcomes, and treatment schedule. Specifically, where available, each patient’s breed, sex, body weight, body condition score, and whether the patient possessed a full-length tail, was recorded. Clinical history information included the age at which the patient was gonadectomized, the age at onset of UI clinical signs, the age at which the patient first presented for treatment, the duration of each patient’s UI clinical signs prior to presentation, the frequency and volume of UI episodes, whether they were currently taking either phenylpropanolamine or diethylstilbesterol, and whether the patient presented primarily to address the UI clinical signs, or if musculoskeletal clinical signs were the primary complaint. Physical examination findings were based on muscle and motion palpation, noting whether there was involvement with any of the lumbar vertebrae or sacro-iliac joints, or associated musculature, including the iliopsoas, iliocostalis, epaxial, sartorius, quadratus lumborum, abdominal wall, adductor, and gracilis muscles. Clinical outcomes examined whether there was a change in either the frequency or volume of UI episodes, and whether the owners reported an improvement in musculoskeletal clinical signs. The treatment schedule noted the total number of appointments, the elapsed time between the initial consult and first recheck appointments, the average time between appointments, time between first and last appointment, and the frequency of UI episodes that followed. A typical examination would consist of history collection followed by a complete orthopaedic examination of each limb, as well as an assessment of spinal cord function. The vertebral column, from the first cervical vertebra to the proximal tail was assessed for altered mobility between adjacent vertebrae, as well as abnormal tone or pain in the surrounding musculature. Manual therapy, including both mobilizations and manipulations, as determined by each patient’s need, was performed as part of the examination itself. Regions of focal muscle hypertonicity affecting vertebral mobility, or focal pain secondary to myofascial trigger points were typical examination findings that were addressed during treatment sessions. Acupuncture using acupoints was routinely performed next, depending on the clinician’s subjective assessment of the patient’s need, and patient’s tolerance of needles. The most commonly used acupoints were LI10 bilaterally, GV14, 8,4, BL 13, 19, 20, 21, 23, 60, ST36 bilaterally, GB34 bilaterally, and KI3. Needles were left in place for up to 10 minutes, but were usually removed earlier, once it was determined that the surrounding muscle tone had normalized. PBM using a class 3b laser (Spectravet lasers, Coeymans Hollow, NY) was applied immediately after acupuncture needle placement. Treatment protocol varied depending on the clinician’s subjective assessment of the patient’s need. Typically, doses were applied for 40 seconds using either a superpulsed (904 nm, 50 mW average, 25 W peak, 18 J/cm2), or continuous wave (810 nm, 500 mW, 20 J/cm2) probe. Any myofascial trigger points that remained following the above treatment were then addressed using dry needling (intramuscular stimulation) techniques. Whenever possible, the treatment goal was to resolve any palpable sources of muscular pain before the treatment session was ended. Statistical analysisDue to high quantities of missing data and the categorical nature of much of the data captured from client files for this analysis, a nonparametric approach was taken with the analysis. Missing data made even this modified approach challenging, so a limited number of questions could be explored using the available data set. The data set was reorganized to facilitate evaluation of a specific a priori hypothesis—we expected to see improvement (i.e., reductions in urine leakage) following treatment. Specifically, each case was examined to determine the frequency (pre- and post-treatment) of UI episodes (daily, weekly, monthly or less frequently), the relative volume of urine for each post-treatment episode relative to the pre-treatment volume (increased, the same, less), and the duration of pre-treatment clinical signs (a month or less, a year or less, more than a year). Chi-square analyses were performed using these categorical variables, sex (neutered males, spayed females), and diagnosis type (USMI, musculoskeletal, both). Spearman’s rho was computed to look at the relationships between key variables, including signalment [history; frequency of leakage (daily, weekly, monthly); medication for USMI; and diagnostic history], physical examination findings, clinical outcomes [change in volume and frequency of leakage (overall, <1 year post treatment, >1 year post- treatment; clinical evaluation of treatment success; musculoskeletal response) and treatment schedules (number and timing of appointments; relapse history) because of the mixed categorical and continuous nature of the variables available, and the large number of missing values on some variables (which limited the number of cases to examine quite dramatically in some cases)]. Ethical approvalThis research conforms to the ethical standards as described by the Canadian Council on Animal Care in science. ResultsThirty-nine patients qualified for the study. Multiple mixed and purebred dog breeds were represented. Body weight averaged 25.3 kg (range 2.7 to 48 kg), and age averaged 8.2 years (range 0.5 to 14 years). Of the qualified patients, 16 dogs were neutered males, 1 was an intact male, and the remaining 22 dogs were spayed females. The age at which the patient was gonadectomized was frequently not noted in the medical record. Similarly, the patient’s age at the time UI clinical signs first appeared, and/or the length of time between onset of clinical signs and the first appointment was indiscernible for multiple patients. At presentation, 10 identified UI as their primary complaint, 9 listed musculoskeletal issues, and the remaining 20 cited both UI and musculoskeletal issues equally, as their primary reason for seeking treatment. No difference in physical examination findings or treatment response was found between these groups. At the time of treatment, 11 patients were taking medication for UI, but were still experiencing breakthrough UI. Six were taking diethylstilbestrol, 4 were taking phenylpropanolamine, and 1 was taking both diethylstilbestrol and phenylpropanolamine. All patients showed some degree of lumbopelvic hypomobility as a physical examination finding. No attempt was made in the medical record to subjectively categorize the severity of pain symptoms demonstrated during examination. Rather, the medical notes recorded the location of reduced vertebral mobility, and among the distinctly palpable muscles, which ones had abnormal tone or myofascial trigger points. All patients received CAMT. Six patients did not receive PBM. The reason for not applying PBM for those patients was because they were part of a larger study examining the efficacy of CAMT as a sole therapy, and therefore were ineligible to receive PBM. All treatments were performed by the same clinician (David Lane). Although the multifactorial nature of this study, and the small number of dogs makes it difficult to draw a conclusion, there appears to be support for the notion that treatment for LBP was associated with a decrease in the owner-reported frequency and volume of UI episodes. To test the hypotheses, data were scrutinized in two ways. Frequency pre- and post-treatment was coded as occurring either daily, weekly, or monthly (or less than monthly). The number of cases available for analysis was 27. Because of a very small number of cases falling into the monthly + less than monthly category, the categories were further collapsed to compare only daily and weekly + less frequent leaking episodes. Next, the data were rearranged to allow a determination of whether the post-treatment frequency for each case was unchanged or decreased compared to pre-treatment frequency (no reports of increases in frequency were observed in the data set). The resulting pattern of results are shown in Table 1. A Chi-square test confirmed that treatment was successful in reducing the frequency of incontinence behaviours (leaking) overall, C21=6.91, p < 0.01. No sex difference in post-treatment leakage volume was observed (C21=0.36, p > 0.05). Across all measured diagnostic categories, however, reduced post-treatment leakage volume was evident as shown in Table 2. A Chi-square test indicated that dogs in all categories appear to have benefitted from treatment insofar as dogs in all diagnostic categories considered experienced reduced leakage volume post treatment, C22=9.44, p < 0.01. The data available to test the hypotheses regarding the impact of treatment on both frequency and volume of leakage were somewhat problematic for a couple of reasons. Although most owners were able to quantify the frequency of UI, some could not. For example, the owner might have been able to detect a urine smell on the dog’s blanket, but could not say if the frequency of leakage leading to that smell was occurring daily, or weekly. Other owners would report urinary leakage if they failed to take certain husbandry practises, such as ensuring the dog urinated shortly before bedtime. Thus, the frequency of UI episodes varied, depending on how well they were able to implement these husbandry measures. At the pre-treatment stage, 35 (89%) owners were able to quantify the frequency of UI, but 3 owners (8%) were not, and 1 (3%) owner only noted UI if they lapsed in their husbandry practises. Post-treatment, 34 (87%) owners were able to quantify the frequency of UI. Table 1. Daily and weekly results.
Table 2. Post-treatment leakage volume.
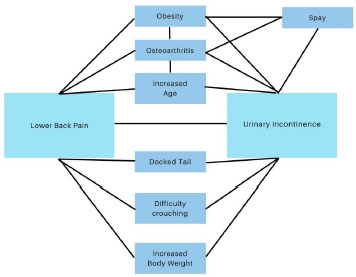
At the post-treatment stage, 38 owners (97%) were able to comment on whether the frequency of UI had changed. Of those, 29 (74%) reported a decrease in the frequency of UI, 9 (23%) reported no change in the frequency of UI, and 0 (0%) reported an increase in frequency. The degree of response varied: 12/38 (32%) reported a reduction but incomplete resolution of clinical signs; that UI episodes decreased in frequency but still occurred at least once a month. 10/38 (28%) reported UI episodes occurred less frequently than once a month, and 7 (18%) reported episodes happening less frequently than once a year. Follow-up assessment greater than a year following the start of treatment was available for only 16/38 (42%) of patients. Attempts had been made to quantify the volume of urine voided during UI episodes by having the owners describe the urine volume on a 0–100 scale, with 0 representing no urine, and 100 representing the volume of a full bladder. Many clients found themselves unable to answer that question retrospectively, instead choosing descriptive terms such as “dribbles,” “small puddle,” etc., In general, clients found it easier to record the frequency of UI episodes relative to the volume voided. 9/39 (23%) owners were unable to make any comment on the volume voided per UI episode (but were able to measure the frequency), whereas only 1/39 (3%) of owners were able to comment on the volume, but not the frequency. Despite not being able to comment on the volume voided per UI episode, 37/39 owners were still able to determine if the global volume of urine leaked changed over time. 27/39 (69%) of owners reported a decrease in urine volume leaked within 8 days of a second treatment, 9/39 (23%) reported no change in urine volume leaked, one owner (3%) reported an increase in urine volume leaked, and the remaining 2/39 (5%) were unable to make a determination. Signalment, history, physical examination findings, outcomes, and treatment schedules were examined using nonparametric correlations (Spearman’s rho). Many significant relationships were identified, but no systematic relationships that would clarify the chi-square findings were observed. DiscussionFollowing treatment of LBP with CAMT, with or without PBM, patients that presented with a clinical history of USMI saw a significant reduction in both frequency and volume of UI episodes. These findings suggest that LBP and USMI are related conditions, and that the clinical signs of USMI can be reduced or eliminated by treating LBP. By extension, these findings also suggest that UI is potentially a previously unrecognized pain symptom. In humans, it is recognized that lumbar hypomobility can occur without pain (Fritz et al., 2007). Because canines are unable to verbally describe their experience, in cases where lumbar hypomobility is detected without any concurrent pain indicators such as avoiding palpation, flinching, head turning, vocalization, etc., it is uncertain if they are experiencing true LBP or non-painful hypomobility. No effort was made to distinguish between these 2 conditions in the medical record, so no data could be collected on whether species specific pain signals were observed. However, hypomobility was recorded, and occurred in all patients. Because treatment was initiated without a requirement for magnetic resonance imaging (MRI) imaging, it cannot be absolutely stated that all the research subjects were experiencing NSLBP, and not mechanical back pain. Similarly, not all patients had received an appropriate workup to distinguish USMI from other causes of UI such as infection, or to rule out other confounding variables such as a pelvic bladder. Future research should consider MRI imaging to rule out mechanical back pain, and standardized diagnostic testing to rule out other potential causes of UI. The fact that morbidities beyond USMI or NSLBP may have been present, might have affected outcomes. Although CAMT, with or without PBM, appears to be an effective treatment for USMI, it is uncertain which of these three modalities are exerting an effect, or if a multimodal approach results in an additive, or even symbiotic, benefit. In humans, some research indicates that each of these modalities has individual benefit in addressing UI. No research on CAMT, with or without PBM for resolving human UI was found. In humans, two manual therapy treatments worked for a minority of patients, with a total of eight treatments given to determine effectiveness (Zhang et al., 2006). Similarly, 10 to 36 acupuncture sessions were administered in order to achieve a clinical response (Shen et al., 2019; Sun et al., 2020). In this paper, the canine patients receiving CAMT, with or without PBM, frequently responded with only two treatments. The faster response rate reported in these dogs, relative to the human population, could reflect a species-specific difference, or possibly a benefit of using a multimodal approach, relative to the use of a single therapy. Further research is required in both species in order to make this determination. Research has shown that female dogs are diagnosed 3–5 times as frequently as males (Coit et al., 2008; Hall et al., 2019; Reichler, 2009; Chew et al., 2011; Byron et al., 2017), yet in this paper, 41% of the subjects were male. The reason for the increased representation of males is unknown. One possible explanation is that male dogs are less likely to respond to conservative therapy (Chew et al., 2011), and the selection criterion of this paper included uncontrolled USMI. Therefore, more females with a diagnosis of USMI may have presented, but because their clinical signs were controlled by medication, they were ineligible to participate in this research. This would create a selection bias toward males, and thus explain their overrepresentation in this paper. Differences exist between male and female dogs in both the underlying cause, and response to treatment, of USMI (Aaron et al., 1996; Hoelzler and Lidbetter, 2004; Coit et al., 2008; Chew et al., 2011; Hall et al., 2019). In this study, we observed no difference in treatment response between male and female dogs. Although this paper did not identify variables that indicate how LBP and USMI might interrelate, elsewhere in the literature multiple authors have identified risk factors for USMI that also correlate with a diagnosis of LBP. In canines, De Bleser et al. (2011) found a strong correlation between a diagnosis of USMI and owners reporting their dog having difficulty assuming a normal urination stance. Inability to assume a normal physiologic posture is a strong indicator of underlying pain and/or abnormally reduced spinal flexibility, consistent with LBP or hypomobility. Furthermore, De Bleser et al. (2011) correlated USMI with a diagnosis of OA, although the location of the OA was never specified. OA of the lumbar facets is a recognized cause of LBP. OA of the hindlimbs also predisposes patients to secondary LBP (Balagué et al., 2012). These correlations were incidental to the primary hypothesis of De Bleser et al.’s (2011) research, but do serve as independent corroborating evidence that a relationship exists between the diagnosis of UI and concurrent musculoskeletal disease. Multiple researchers have reported that UI is associated with having a docked tail, but no reason for this correlation has been determined (Holt and Thrusfield, 1993; Wansbrough, 1996; de Bleser et al., 2011). Anatomically, the musculature of the tail is continuous with the perianal region, pelvic diaphragm and lumbar musculature, and physiologically aids in a dog’s ability to jump, turn corners at speed, negotiate narrow structures, and climb (Wansbrough, 1996; Patel and Braae, 2013; Zink and Van Dyke, 2018). Docking the tail leads to atrophy of this musculature and subsequent weakening of the pelvic diaphragm and lumbosacral musculature (Wansbrough, 1996). Inadequate muscle strength has been linked to an increase in both acute and repetitive stress injury in people (Lauersen et al., 2014). Thus, a docked tail may predispose to LBP in dogs, which in turn may give rise to UI. The relationship between obesity, USMI, gonadectomy status, sex, body weight, age, OA, and LBP, is complex (Fig. 1). In people, obesity is a risk factor for both OA and NSLBP (Smith et al., 2006). In dogs, obesity has been linked to OA, and the severity of OA (Frye et al., 2016). OA is correlated with USMI in dogs (de Bleser et al., 2011). OA is a risk factor for LBP (De Decker et al., 2014). Gonadectomized females are more likely to become obese (Simpson et al., 2019). A relationship between obesity and USMI also exists (Hall et al., 2019). Middle-aged spayed females are most likely to be obese, and advancing age is also a risk factor for USMI (Hall et al., 2019; Simpson et al., 2019). Advancing age is also correlated with degenerative back disease and LBP in dogs (Henderson et al., 2015; Worth et al., 2019). In humans, degenerative lower back disease is frequently preceded by NSLBP. Dogs gonadectomized before 6 months of age are also at an increased risk for OA, in addition to obesity (Simpson et al., 2019).
Fig. 1. Relationship between risk factors for USMI and LBP. Increasing body weight, with or without obesity, is linked to USMI in females, but not in males (Hall et al., 2019). Increasing body weight is also linked to degenerative lumbar disease (Worth et al., 2019). Spayed females are more likely to be obese compared to neutered males. Unlike spayed versus intact females, neutered males may not be predisposed to USMI when compared to intact males (Hall et al., 2019). It will take considerable research to separate the relationship between these intertwined variables to see whether they exert an independent effect on the incidence of USMI. Each sex should be examined separately. Both lumbosacral degenerative disease and UI is more prevalent in older dogs (de Bleser et al., 2011; Reichler and Hubler, 2014; Henderson et al., 2015; Hall et al., 2019; Pegram et al., 2019; Worth et al., 2019). In humans, it has been shown that radiographic evidence of degenerative lumbosacral disease is often preceded by NSLBP. One possible explanation for delay in onset of USMI until years after being gonadectomized, is that it is not until the cumulative effect of both a gonadectomy and age-related LBP, that the patient begins experiencing clinical UI. Alternatively, it may be that LBP is the primary cause of USMI in a given patient, and the gonadectomy is incidental. The multifactorial nature of USMI may also explain the variable response to treatment seen among dogs. Dogs for whom the LBP was an incidental finding not contributing to UI, would be expected to show no improvement at all. Conversely, patients for whom the LBP is the primary or exclusive cause of UI, might show a complete response. The nature of the LBP itself may also contribute to the variable clinical responses reported. Dogs with an acute muscular injury and no underlying chronic pathology, such as degenerated intravertebral discs or OA, may show a permanent response to one or two treatments if the LBP was the primary or exclusive cause of the UI. Dogs with permanent underlying pathology such as degenerated intravertebral discs or OA, may be prone to recurrence of the LBP despite an initial response to treatment. Such cases may be reflected in the patients that required repeated treatments every few months in order to prevent relapse of UI clinical signs. It is unknown whether LBP or hypomobility is an actual cause of USMI. If it is a cause, then the underlying physiologic mechanism is also speculative. Possible explanations include hypertonic muscle impinging upon, or constricting blood flow to, the pudendal nerve, causing secondary paresis and reduced urethral tone. Alternatively, as suggested by Thude (2015), NSLBP could “interact with sympathetic innervation of the bladder as a mechanism” behind UI (Thude, 2015). Both these mechanisms can be occurring concurrently. Further physiologic testing, such as measuring urethral and cystic pressure, is required to determine if the relationship between LBP and USMI is causal, and if so, to determine the underlying mechanism. This study is limited by its retrospective nature. Future blinded prospective randomized controlled clinical therapeutic trials are needed to confirm results. Gaps in the medical records could be remedied by providing standardized questionnaires to clients. Additional information could also be recorded, for instance to determine if overnight UI episodes relate to a history of increased exercise the previous day. Therapeutic effect could be further quantified by measuring physiologic parameters such as urethral and cystic pressure, electromyelography, and measuring residual urine volume, pre and post treatment. If future research substantiates the findings of this limited case review study, it may fundamentally change our approach to assessing and treating USMI. Because chronic pain is a welfare issue, every patient presenting with a history of UI should be assessed for both LBP and hypomobility. If LBP or hypomobility is detected, then it should be resolved as a part of the primary therapeutic approach, before assessing the need for chronic pharmaceutics, and/or surgical intervention. Conflict of interestThe authors declare that there is no conflict of interest. Authors’ contributionDavid M. Lane: conceptualization, data collection, primary author. Sarah A. Hill: statistical analysis, edits. ReferencesAaron, A., Eggleton, K., Power, C. and Holt, P.E. 1996. Urethral sphincter mechanism incompetence in male dogs: a retrospective analysis of 54 cases. Vet. Rec. 139, 542–546; doi:10.1136/vr.139.22.542 Balagué, F., Mannion, A.F., Pellisé, F. and Cedraschi, C. 2012. Non-specific low back pain. Lancet 379, 482–491; doi:10.1016/S0140-6736(11)60610-7 Byron, J.K., Taylor, K.H., Phillips, G.S. and Stahl, M.S. 2017. Urethral sphincter mechanism incompetence in 163 neutered female dogs: diagnosis, treatment, and relationship of weight and age at neuter to development of disease. J. Vet. Intern. Med. 31, 442–448; doi:10.1111/jvim.14678 Chew, D.J., DiBartola, S.P. and Schenck, P.A. 2011. Chapter 13—Disorders of micturition and urinary incontinence. In Canine and feline nephrology and urology, 2nd ed. Saint Louis, MI: W.B. Saunders, pp: 409–433; doi:10.1016/B978-0-7216-8178-8.10013-2 Coit, V.A., Gibson, I.F., Evans, N.P. and Dowell, F.J. 2008. Neutering affects urinary bladder function by different mechanisms in male and female dogs. Eur. J. Pharmacol. 584, 153–158; doi:10.1016/j.ejphar.2008.02.037 de Bleser, B., Brodbelt, D.C., Gregory, N.G. and Martinez, T.A. 2011. The association between acquired urinary sphincter mechanism incompetence in bitches and early spaying: a case-control study. Vet. J. 187, 42–47; doi:10.1016/j.tvjl.2009.11.004 De Decker, S., Wawrzenski, L.A. and Volk, H.A. 2014. Clinical signs and outcome of dogs treated medically for degenerative lumbosacral stenosis: 98 cases (2004–2012). J. Am. Vet. Med. Assoc. 245, 408–413; doi:10.2460/javma.245.4.408 Eliasson, K., Elfving, B., Nordgren, B. and Mattsson, E. 2008. Urinary incontinence in women with low back pain. Man. Ther. 13, 206–212; doi:10.1016/j.math.2006.12.006 Flynn, T., Fritz, J., Whitman, J., Wainner, R., Magel, J., Rendeiro, D., Butler, B., Garber, M. and Allison, S. 2002. A clinical prediction rule for classifying patients with low back pain who demonstrate short-term improvement with spinal manipulation. Spine 27, 2835–2843; doi:10.1097/00007632-200212150-00021 Forsee, K.M., Davis, G.J., Mouat, E.E., Salmeri, K.R. and Bastian, R.P. 2013. Evaluation of the prevalence of urinary incontinence in spayed female dogs: 566 cases (2003–2008). J. Am. Vet. Med. Assoc. 242, 959–962; doi:10.2460/javma.242.7.959 Fritz, J.M., Cleland, J.A. and Childs, J.D. 2007. Subgrouping patients with low back pain: evolution of a classification approach to physical therapy. J. Orthop. Sports Phys. Ther. 37, 290–302; doi:10.2519/jospt.2007.2498 Frye, C.W., Shmalberg, J.W. and Wakshlag, J.J. 2016. Obesity, exercise and orthopedic disease. Vet. Clin. North Am. Small Anim. Pract. 46, 831–841; doi:10.1016/j.cvsm.2016.04.006 Ghaderi, F., Mohammadi, K., Amir Sasan, R., Niko Kheslat, S. and Oskouei, A.E. 2016. Effects of stabilization exercises focusing on pelvic floor muscles on low back pain and urinary incontinence in women. Urology 93, 50–54; doi:10.1016/j.urology.2016.03.034 Hall, J.L., Owen, L., Riddell, A., Church, D.B., Brodbelt, D.C. and O’Neill, D.G. 2019. Urinary incontinence in male dogs under primary veterinary care in England: prevalence and risk factors: Urinary incontinence in male dogs. J. Small Anim. Pract. 60, 86–95; doi:10.1111/jsap.12951 Henderson, A.L., Hecht, S. and Millis, D.L. 2015. Lumbar paraspinal muscle transverse area and symmetry in dogs with and without degenerative lumbosacral stenosis: paraspinal muscle and lumbosacral stenosis in dogs. J. Small Anim. Pract. 56, 618–622; doi:10.1111/jsap.12385 Hoelzler, M.G. and Lidbetter, D.A. 2004. Surgical management of urinary incontinence. Vet. Clin. North Am. Small Anim. Pract. 34, 1057–1073; doi:10.1016/j.cvsm.2004.03.003 Holt, P.E. and Thrusfield, M.V. 1993. Association in bitches between breed, size, neutering and docking, and acquired urinary incontinence due to incompetence of the urethral sphincter mechanism. Vet. Rec. 133, 177–180; doi:10.1136/vr.133.8.177 Lane, D.M. and Hill, S.A. 2016a. Pressure algometry measurement of canine muscular pain near the thoracolumbar junction: evaluation of a modified technique. Vet. Anaesth. Analg. 43, 227–234; doi:10.1111/vaa.12308 Lane, D.M. and Hill, S.A. 2016b. Effectiveness of combined acupuncture and manual therapy relative to no treatment for canine musculoskeletal pain. Can. Vet. J. 57, 407–414. Lauersen, J.B., Bertelsen, D.M. and Andersen, L.B. 2014. The effectiveness of exercise interventions to prevent sports injuries: a systematic review and meta-analysis of randomised controlled trials. Br. J. Sports Med. 48, 871–877; doi:10.1136/bjsports-2013-092538 Mackova, K., Van daele, L., Page, A., Geraerts, I., Krofta, L. and Deprest, J. 2020. Laser therapy for urinary incontinence and pelvic organ prolapse: a systematic review. BJOG Int. J. Obstet. Gynaecol. 127, 1338–1346; doi:10.1111/1471-0528.16273 Millis, D. and Levine, D. 2013. Canine rehabilitation and physical therapy, 2nd ed. Saunders, Philadelphia, Pennsylvania, USA. Patel, A. and Braae, M. 2013. Rapid turning at high-speed: inspirations from the cheetah’s tail. In Presented at the 2013 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS 2013), Tokyo, Japan: IEEE, pp: 5506–5511; doi:10.1109/IROS.2013.6697154 Pegram, C., O’Neill, D.G., Church, D.B., Hall, J., Owen, L. and Brodbelt, D.C. 2019. Spaying and urinary incontinence in bitches under UK primary veterinary care: a case–control study. J. Small Anim. Pract. 60, 395–403; doi:10.1111/jsap.13014 Power, S.C., Eggleton, K.E., Aaron, A.J., Holt, P.E. and Cripps, P.J. 1998. Urethral sphincter mechanism incompetence in the male dog: importance of bladder neck position, proximal urethral length and castration. J. Small Anim. Pract. 39, 69–72; doi:10.1111/j.1748-5827.1998.tb03596.x Reichler, I. 2009. Gonadectomy in cats and dogs: a review of risks and benefits. Reprod. Domest. Anim. 44, 29–35; doi:10.1111/j.1439-0531.2009.01437.x Reichler, I. and Hubler, M. 2014. Urinary incontinence in the bitch: an update. Reprod. Domest. Anim. 49, 75–80; doi:10.1111/rda.12298 Shen, J., Luo, R., Zhang, L., Li, Y., Ke, L. and Gao, Z. 2019. Using electroacupuncture with optimized acupoint positioning to predict the efficacy of sacral neuromodulation of refractory overactive bladder: a case report. Medicine (Baltimore) 98, e17795; doi:10.1097/MD.0000000000017795 Simpson, M., Albright, S., Wolfe, B., Searfoss, E., Street, K., Diehl, K. and Page, R. 2019. Age at gonadectomy and risk of overweight/obesity and orthopedic injury in a cohort of Golden Retrievers. PLoS One 14, e0209131; doi:10.1371/journal.pone.0209131 Smith, M.D., Russell, A. and Hodges, P.W. 2006. Disorders of breathing and continence have a stronger association with back pain than obesity and physical activity. Aust. J. Physiother. 52, 11–16; doi:10.1016/S0004-9514(06)70057-5 Spain, C.V., Scarlett, J.M. and Houpt, K.A. 2004. Long-term risks and benefits of early-age gonadectomy in dogs. J. Am. Vet. Med. Assoc. 224, 380–387; doi:10.2460/javma.2004.224.380 Sun, Y., Liu, Y., Liu, S., Wang, W. and Liu, Z. 2020. Electroacupuncture for women with urgency-predominant mixed urinary incontinence: secondary analysis of a randomized noninferiority trial. World J. Urol. 38, 1035–1042; doi:10.1007/s00345-019-02828-1 Thrusfield, M.V., Holt, P.E. and Muirhead, R.H. 1998. Acquired urinary incontinence in bitches: its incidence and relationship to neutering practices. J. Small Anim. Pract. 39, 559–566; doi:10.1111/j.1748-5827.1998.tb03709.x Thude, T.R. 2015. Chiropractic abnormalities of the lumbar spine significantly associated with urinary incontinence and retention in dogs: chiropractic associated with incontinence. J. Small Anim. Pract. 56, 693–697; doi:10.1111/jsap.12420 Wansbrough, R.K. 1996. Cosmetic tail docking of dogs. Aust. Vet. J. 74, 59–63; doi:10.1111/j.1751-0813.1996.tb13737.x Worth, A., Meij, B. and Jeffery, N. 2019. Canine degenerative lumbosacral stenosis: prevalence, impact and management strategies. Vet. Med. Res. Rep. 10, 169–183; doi:10.2147/VMRR.S180448 Zhang, J., Haselden, P. and Tepe, R. 2006. A case series of reduced urinary incontinence in elderly patients following chiropractic manipulation. J. Chiropr. Med. 5, 88–91; doi:10.1016/S0899-3467(07)60139-6 Zink, M.C. and Van Dyke, J. 2018. Canine sports medicine and rehabilitation, 1st ed. Hoboken, NJ: Wiley. | ||
| How to Cite this Article |
| Pubmed Style Lane DM, Hill SA, . The relationship between urethral sphincter mechanism incompetency and lower back pain: positing a novel treatment for urinary incontinence in dogs. Open Vet J. 2022; 12(1): 105-113. doi:10.5455/OVJ.2022.v12.i1.13 Web Style Lane DM, Hill SA, . The relationship between urethral sphincter mechanism incompetency and lower back pain: positing a novel treatment for urinary incontinence in dogs. https://www.openveterinaryjournal.com/?mno=138654 [Access: April 19, 2024]. doi:10.5455/OVJ.2022.v12.i1.13 AMA (American Medical Association) Style Lane DM, Hill SA, . The relationship between urethral sphincter mechanism incompetency and lower back pain: positing a novel treatment for urinary incontinence in dogs. Open Vet J. 2022; 12(1): 105-113. doi:10.5455/OVJ.2022.v12.i1.13 Vancouver/ICMJE Style Lane DM, Hill SA, . The relationship between urethral sphincter mechanism incompetency and lower back pain: positing a novel treatment for urinary incontinence in dogs. Open Vet J. (2022), [cited April 19, 2024]; 12(1): 105-113. doi:10.5455/OVJ.2022.v12.i1.13 Harvard Style Lane, D. M., Hill, S. A. & (2022) The relationship between urethral sphincter mechanism incompetency and lower back pain: positing a novel treatment for urinary incontinence in dogs. Open Vet J, 12 (1), 105-113. doi:10.5455/OVJ.2022.v12.i1.13 Turabian Style Lane, David M, Sarah A Hill, and . 2022. The relationship between urethral sphincter mechanism incompetency and lower back pain: positing a novel treatment for urinary incontinence in dogs. Open Veterinary Journal, 12 (1), 105-113. doi:10.5455/OVJ.2022.v12.i1.13 Chicago Style Lane, David M, Sarah A Hill, and . "The relationship between urethral sphincter mechanism incompetency and lower back pain: positing a novel treatment for urinary incontinence in dogs." Open Veterinary Journal 12 (2022), 105-113. doi:10.5455/OVJ.2022.v12.i1.13 MLA (The Modern Language Association) Style Lane, David M, Sarah A Hill, and . "The relationship between urethral sphincter mechanism incompetency and lower back pain: positing a novel treatment for urinary incontinence in dogs." Open Veterinary Journal 12.1 (2022), 105-113. Print. doi:10.5455/OVJ.2022.v12.i1.13 APA (American Psychological Association) Style Lane, D. M., Hill, S. A. & (2022) The relationship between urethral sphincter mechanism incompetency and lower back pain: positing a novel treatment for urinary incontinence in dogs. Open Veterinary Journal, 12 (1), 105-113. doi:10.5455/OVJ.2022.v12.i1.13 |